Limb Ataxia Unraveled: Decoding Causes, Symptoms, and Spearheading Treatments
Limb Ataxia Unraveled: Decoding Causes, Symptoms, and Spearheading Treatments
Limb ataxia—characterized by impaired coordination and unsteady gait stemming from neurological dysfunction in the limbs—represents a challenging movement disorder affecting balance, motor precision, and daily function. While often mistaken for isolated clumsiness or coordination issues, limb ataxia is a telltale sign of underlying brain or spinal pathology. Understanding its causes, recognizing its symptoms, and exploring available treatments is essential for early intervention and improved patient outcomes.
This in-depth analysis examines the complex interplay behind limb ataxia, offering a clinical roadmap for both medical professionals and individuals impacted by this disabling condition.
Limb ataxia manifests as inconsistent, jerky, or fluid movement in the arms and legs, often disrupting simple actions like walking, reaching, or holding objects. Unlike general weakness, ataxia specifically reflects a breakdown in motor planning and execution linked to cerebellar or corticospinal pathway damage.
Its complexity arises from multiple neurological sources, requiring careful differentiation to guide effective management. “Ataxia is not a disease itself, but a neurological symptom—like a finger pointing to a wide constellation of possible causes,” explains Dr. Elena Ramirez, a neurologist specializing in movement disorders at the Cleveland Clinic.
Pinpointing the root cause is the cornerstone of targeted therapy.
Unmasking the Roots: Key Causes of Limb Ataxia
Limb ataxia stems from diverse neurological insults, broadly categorized as neurological, genetic, metabolic, or structural. The cerebellum, brainstem nuclei involved in motor control, or descending corticospinal tracts can all be compromised.Major causes include:
Metabolic derangements—especially thiamine deficiency in conditions like Wernicke’s encephalopathy—disrupt neurologic function, often reversing with prompt vitamin therapy.
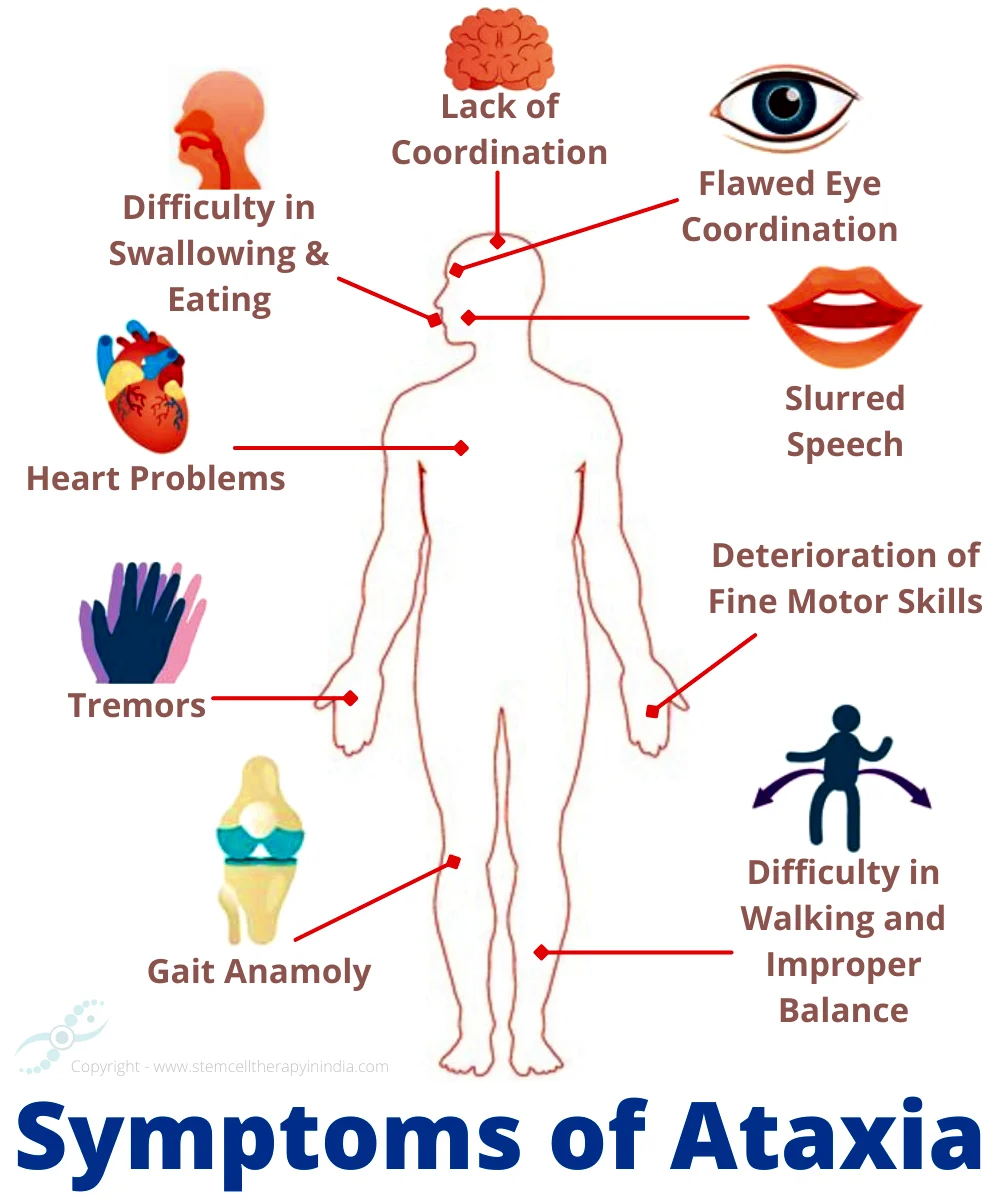
While symptoms vary in onset and severity, limb ataxia consistently disrupts motor harmony. Patients frequently report:
- A shuffling, irregular gait with frequent stumbling, even on flat surfaces.
- Unsteadiness while performing fine motor tasks—like buttoning a shirt or holding a pencil.
- Difficulty with rhythmic or precise movements, such as tapping a finger or walking heel-to-toe.
- Poor balance in darkness or uneven terrain, underscoring deficits in sensory integration alongside motor control.
- In progressive cases, worsening clumsiness and increasing assistance required for mobility.
Diagnosing limb ataxia begins with a detailed clinical history and neurological examination, focusing on the timing, progression, and pattern of motor disturbances. A meticulous approach identifies red flags: rapid onset may point to stroke, while gradual development suggests genetic or metabolic origin. Advanced imaging—and in select cases, genetic testing—plays a pivotal role.
Imaging Studies: MRI of the brain and spinal cord is the cornerstone, revealing cerebellar atrophy, tumors, or stroke-related lesions.
Functional imaging, including PET or SPECT, aids in metabolic or inflammatory assessments.
Genetic and Metabolic Testing: For suspected hereditary ataxias, genetic panels target specific conditions such as SCA genes. Blood tests screen for thiamine levels, vitamin deficiencies, or markers of autoimmune or metabolic dysfunction.
electrodiagnostic Tests: While electromyography (EMG) and nerve conduction studies rarely detect ataxia itself, they help rule out concurrent peripheral neuropathies, ensuring focus remains on central nervous system pathology.
Effective management hinges on identifying and addressing the underlying cause—when possible—while supporting motor function through multidisciplinary care. Treatment strategies vary widely, ranging from metabolic correction to immune modulation and symptomatic relief.
Metabolic Correction: For cases linked to vitamin deficiencies (e.g., folate, B12), or thiamine-responsive conditions like Wernicke’s encephalopathy, prompt supplementation often normalizes ataxic symptoms.
Early intervention is critical, as irreversible damage may set in without timely care.
Disease-Modifying Therapies: In genetic ataxias such as SCA, research into antisense oligonucleotides and neuroprotective agents offers hope for slowing progression. Though no cure exists for


Related Post

Decoding Mercedes Benz P0000: Unlocking the Code for Spark Plug Cluster Insights

Understanding Atpl Brain Disease Causes Symptoms And Treatment

How Much Does a CVS Flu Shot Cost? The Shocking Truth — and Why Now’s the Time to Know Before It’s Too Late
Tiny Red Spots on Eyelids: Unraveling the Causes, Symptoms, and Remedies

