What Is PTSD? Understanding the Meaning, Mechanisms, and Symptoms
What Is PTSD? Understanding the Meaning, Mechanisms, and Symptoms
Post-Traumatic Stress Disorder (PTSD) is a complex and often misunderstood mental health condition triggered by experiencing or witnessing life-threatening events. Far from a simple reaction to stress, PTSD reshapes brain function and perception, leaving lasting psychological imprints that disrupt daily life. Its impact reaches beyond emotional distress, influencing cognitive ability, relationships, and physical well-being—making awareness of its meaning and symptoms essential for timely intervention and support.
Understanding PTSD begins with recognizing its roots in trauma. The disorder emerges in the aftermath of events such as combat exposure, natural disasters, assault, serious accidents, or other experiences that profoundly threaten survival. According to the American Psychological Association, PTSD is not a sign of weakness but a testament to the brain’s struggle to process overwhelming sensory and emotional input.
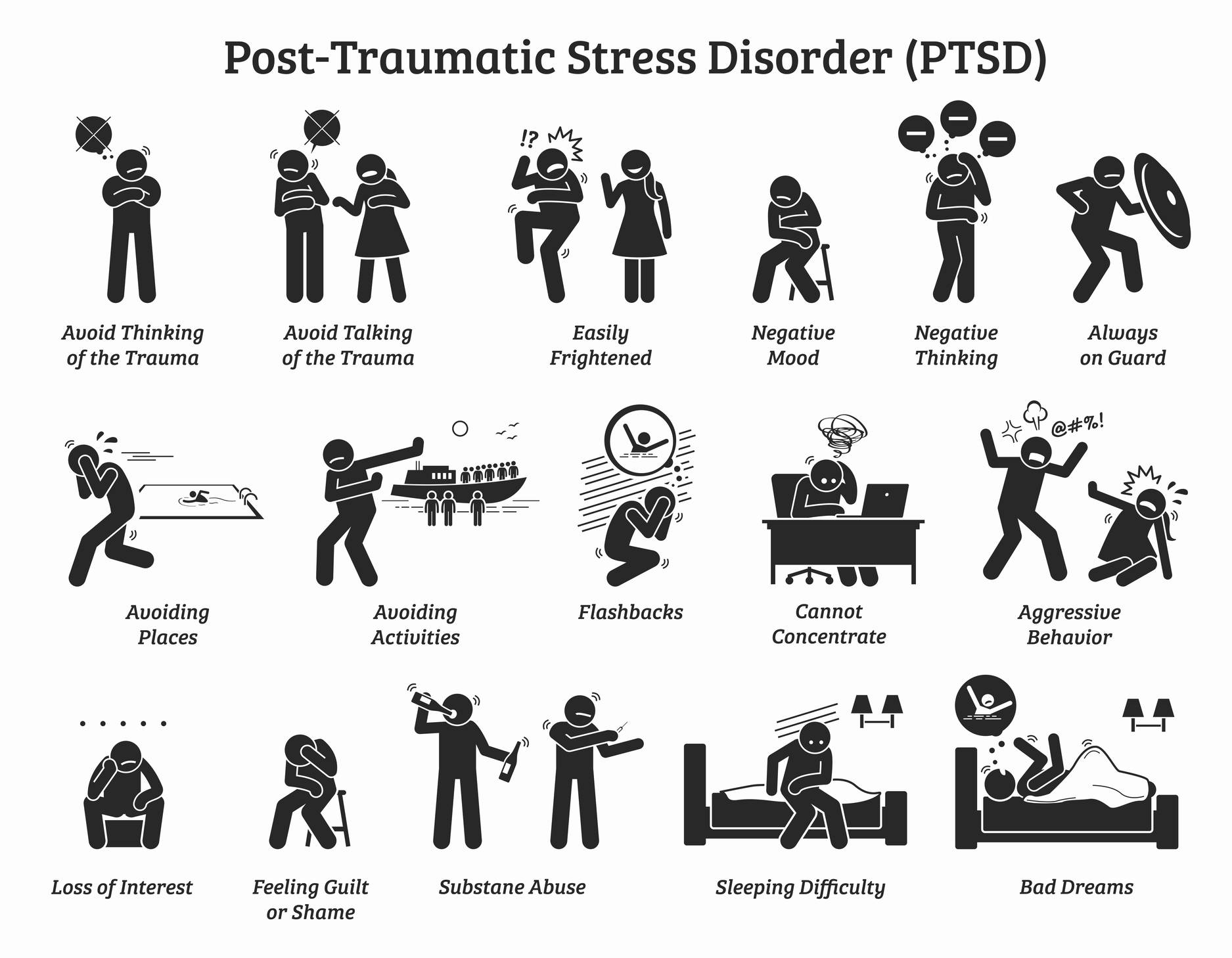
As Dr. Matthew Brown, a clinical psychologist specializing in trauma, explains, “PTSD develops when the mind gets ‘stuck’ in fear, replaying the trauma as if it is happening again.” This fundamental shift transforms a singular frightening event into a persistent psychological burden. Symptoms of PTSD are categorized into four primary clusters—re-experiencing, avoidance, negative alterations in mood and cognition, and hyperarousal—each reflecting distinct neurological and behavioral changes.
### Re-experiencing: The Mind’s Uncontrollable Reliving A hallmark of PTSD is the involuntary re-experiencing of the traumatic event, often through vivid flashbacks, intrusive memories, or distressing dreams. These episodes blur the boundary between past and present, triggering intense emotional and physiological responses as if the danger were imminent. Consider the soldier flashing back to gunfire in a battlefield or the survivor reliving a violent assault flash-forward in a night parade—such intrusions are not signs of flakiness, but neurological flashbacks hardwired by trauma.
- Intense, recurrent distress when exposed to trauma-related reminders - Flashbacks involving vivid sensory details (sights, sounds, smells) - Nightmares interrupting rest and recurring themes of fear These re-experiencing symptoms can feel overwhelming, pulling individuals out of the present moment and trapping them in cycles of distress. ### Avoidance: Protecting the Mind at All Costs To reduce suffering, many individuals with PTSD engage in avoidance behaviors—steering clear of people, places, or activities that trigger memories. This adaptive-response turns restrictive, limiting meaningful engagement with life.
For example, a trauma survivor might stop driving after a near-collision, or avoid social gatherings that recall past vulnerability. Avoidance may offer temporary relief but deepens isolation and impedes healing. ### Negative Changes in Mood and Cognition PTSD reshapes emotional and cognitive patterns, often manifesting as diminished interest in former joys, feelings of detachment from others, or persistent negative beliefs such as “the world is unsafe” or “I am broken.” These cognitive shifts are not signs of personal failure but disruptions in how trauma alters brain function—particularly in regions managing emotion regulation, memory, and self-perception.
Over time, this internal narrative can harden into a chronic outlook, further isolating the individual. Dr. Sarah Lin, a neuroscientist studying trauma’s impact on memory, notes, “Trauma imprints itself not just as a memory, but as a deeply felt emotional state.
The brain remembers how danger felt, more than what actually occurred.” This distinction underscores why PTSD symptoms persist long after the threat has passed—the mind continues to perceive danger in familiar environments or triggers. ### Hyperarousal: Living on Edge Always Hyperarousal reflects a heightened state of physiological readiness known as chronic hypervigilance. Individuals may experience exaggerated startle responses, insomnia, irritability, or an unshakable sense of danger.
The nervous system remains locked in “fight-or-flight,” draining energy and increasing vulnerability to anxiety, anger, and fatigue. What begins as a protective mechanism becomes exhausting, coloring every interaction with unease. A veteran, for instance, might be startled by a car backfire, not from the sound itself, but because their brain interprets it as gunfire.
Such chronic stress impacts not only mental health but cardiovascular function and immune response, illustrating PTSD’s systemic reach. Understanding the full scope of PTSD’s symptoms reveals a condition deeply rooted in neurobiology and psychology. Left untreated, these symptoms can erode resilience, diminish quality of life, and raise risks for comorbid conditions like depression and substance use.
Yet effective interventions—from evidence-based psychotherapies like Cognitive Processing Therapy and Prolonged Exposure, to targeted medications and emerging trauma-informed practices—offer pathways to recovery. Recognizing PTSD requires compassion and clarity, not stigma. It is not a personal flaw but a human response to abnormal stress, demanding informed support rather than judgment.
As research advances, so too does the capacity to validate survivors’ experiences, break down misconceptions, and foster healing environments where recovery is not just possible—but inevitable.


Related Post

Top Sports TV App Transforms Viewing with Unmatched Access to Games & Highlights
Tv.Youtube.Com/Start: Seamless Activation for YouTube TV

Better For You – Siopaolo: Seberang Gitu Lirik, Arti Terjemahan dan Et Fearkan Dalam Budaya Filipina

