What Is an Etiological Model in CBT for Addiction? Unraveling the Root Causes Behind Compulsive Behavior
What Is an Etiological Model in CBT for Addiction? Unraveling the Root Causes Behind Compulsive Behavior
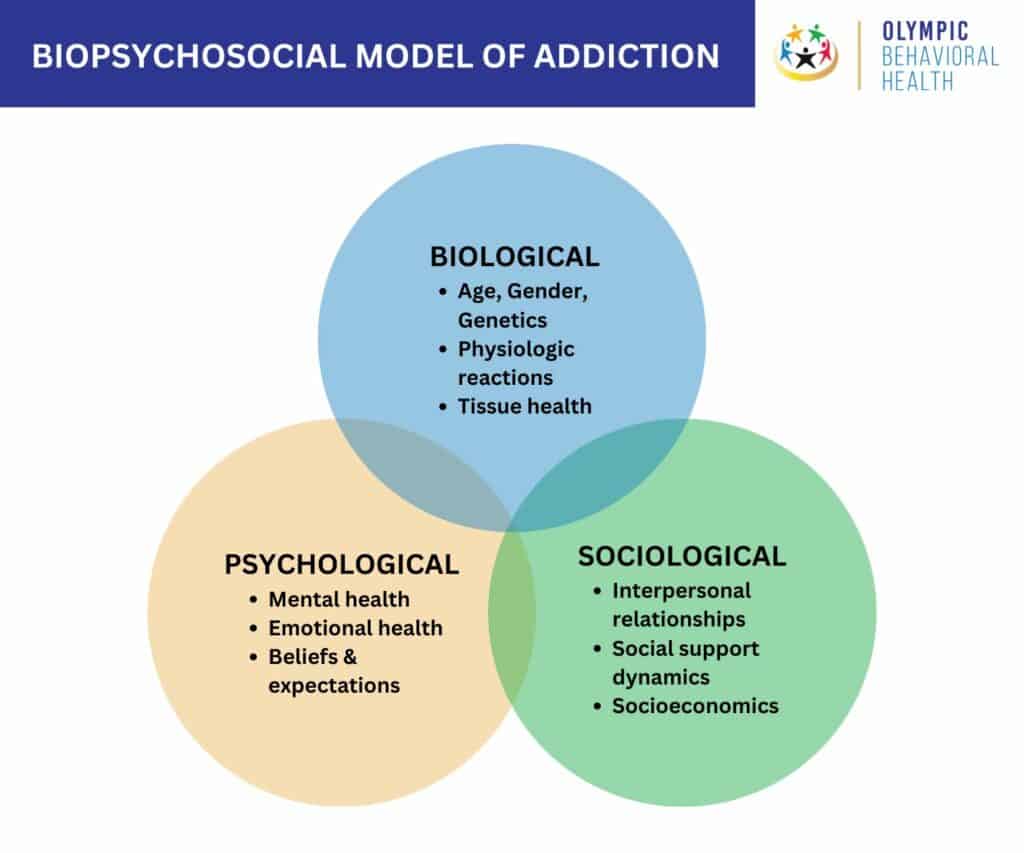
Understanding addiction requires more than observing patterns of drug use or alcohol dependence—it demands a deep dive into *why* these behaviors take hold. At the heart of modern psychological intervention lies the etiological model in cognitive behavioral therapy (CBT), a framework that identifies and dissects the root causes fueling addictive cycles. This model shifts focus from mere symptoms to the psychological, biological, and environmental forces driving substance use, offering clinicians a precise compass to guide treatment.
By mapping out causal pathways, CBT’s etiological model transforms abstract addiction into actionable insights, empowering both patients and therapists to confront the lived experience behind each relapse. ## The Foundations of CBT’s Etiological Framework Cognitive Behavioral Therapy rests on the principle that thoughts, feelings, and behaviors are deeply interconnected—and that addictive behaviors often stem from learned cognitive distortions and maladaptive coping mechanisms. The etiological model in CBT addiction specifically seeks to uncover what triggers and sustains substance use, integrating principles from behavioral psychology, neuroscience, and trauma theory.
As psychologist Michael Miller explains, “Addiction is rarely about the substance itself; it’s about unresolved needs, discomfort, or negative emotional states that the individual tries to escape.” This shift reframes addiction not as moral failure but as a learned response to pain. Key components of the model include: - **Biological predispositions**: Genetic vulnerability, brain reward system sensitization, and neurochemical imbalances that increase susceptibility to addiction. - **Psychological factors**: Co-occurring mental health disorders such as anxiety, depression, or post-traumatic stress, which often coexist with substance use as self-medication.
- **Learning and conditioning**: Environmental cues, social reinforcement, and repeated behavioral patterns that condition the brain to associate substances with relief or reward. - **Developmental context**: Early life stressors, trauma, or dysfunctional family dynamics that shape coping strategies and emotional regulation. These elements interact dynamically, creating complex, individualized pathways into addiction—no single cause dominates, but multiple converging influences sustain it.
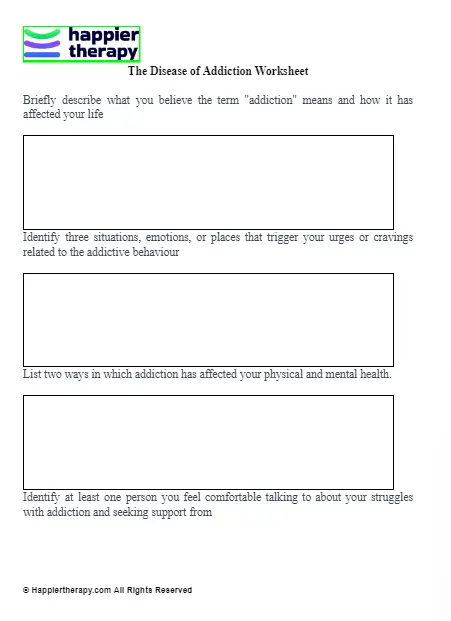
## Mapping the Pathways: How CBT Identifies Causal Links In CBT practice, identifying etiology is not a speculative exercise but a structured process grounded in clinical assessment. Therapists employ tools like detailed interviews, behavioral tracking, and cognitive profiling to trace how past experiences influence present behavior. This process typically unfolds in stages, beginning with identifying triggers and progressing to uncovering underlying beliefs and emotional drivers.
- **Trigger Identification**: Clients are guided to recognize specific environmental, emotional, or social cues that precede substance use. These triggers—ranging from stress at work to social boredom—become focal points for intervention. - **Cognitive Pattern Analysis**: Through cognitive restructuring, clients learn to detect distorted thinking patterns, such as all-or-nothing beliefs or emotional reasoning, that justify use.
“I feel worthless, so a drink helps me relax,” becomes unpacked and challenged. - **Behavioral Experimentation**: Clients test new responses to triggers in controlled settings, learning that relief can be achieved without substances. Over time, alternative behaviors replace automatic cravings.
- **Trauma and Emotional History**: Particularly in cases involving past abuse or neglect, therapists address unresolved trauma, which often fuels addiction as a form of numbing or dissociation. This systematic deconstruction turns addiction’s opacity into transparency. By mapping the sequence from stress to use to consequence, CBT provides a narrative that patients can understand, own, and disrupt.
## Practical Applications: Etiological Insights in Action Real-world CBT programs illustrate the power of the etiological model. In a study from the Journal of Addictive Diseases, clients with opioid use disorder underwent CBT that began with identifying conditioned triggers—such as visits to old neighborhoods—followed by examining how these sites tied to memories of pain or loss. Once triggers were mapped, therapists integrated cognitive restructuring to challenge beliefs like “I can’t handle this feel.” Concurrent trauma-informed techniques helped process unresolved grief, reducing the emotional urgency to use.
Another example lies in substance use among adolescents. Research shows that teens with anxiety often start drinking to manage social stress, a pattern reinforced by brief social rewards. CBT helps reframe this by building healthy coping skills—deep breathing, assertiveness training—while gradually reducing avoidance behaviors.
The etiological model thus tailors treatment to what *causes* the behavior, rather than suppressing symptoms. Importantly, relapse prevention hinges on maintaining awareness of these underlying causes. When a client understands their unique etiological triggers—say, springtime seasonal stress or loneliness—they gain agency to respond mindfully instead of reacting impulsively.
This insight is empowering, fostering self-efficacy and long-term resilience. ## Challenges and Criticisms: Limitations of the Etiological Model Despite its strengths, the CBT etiological model is not without constraints. Critics note that biological factors—such as dopamine receptor variations or epigenetic influences—are complex and often underrepresented in behavioral-only frameworks.
The model’s emphasis on learnable behaviors may inadvertently minimize the profound neurological rewiring that addiction entails, potentially oversimplifying chronic cases. Furthermore, cultural and socioeconomic variables—like systemic inequities, access to treatment, or stigma—are not always fully integrated, risking a narrow focus on individual cognition over broader contextual forces. Yet, proponents counter that CBT’s flexibility allows integration of biological insights through medication collaboration and trauma-informed care.
When combined with neurobiological research, the model grows richer, acknowledging both brain chemistry and learned behavior. This evolution ensures the etiological framework remains relevant amid emerging scientific discoveries. ## The Future of CBT’s Etiological Model: Toward Personalized, Integrative Care As addiction science advances, the etiological model in CBT continues to evolve toward greater personalization and integration.
Machine learning algorithms now help analyze vast datasets to predict individual risk profiles based on genetics, environment, and behavior patterns. Digital therapeutics offer real-time tracking of triggers and mood, enabling proactive interventions. Meanwhile, collaborative care models bring together CBT therapists, psychiatrists, and social workers to address not just behavior but holistic well-being.
This movement toward integration enhances treatment precision. A person with alcohol dependence triggered by work stress and a history of childhood neglect receives a plan that combines CBT for thought restructuring, trauma therapy to process past pain, and stress management skills. In such a model, no factor is ignored—cognition, emotion, biology, and context all converge.
Understanding addiction through a CBT etiological lens transforms it from a static diagnosis into a dynamic process—one rooted in human experience systems informed by science. By identifying what causes each person’s struggle, therapy becomes a targeted journey of healing, not just containment. As clinical practice matures, the model’s clarity and adaptability position it at the forefront of compassionate, effective addiction treatment—proving that sustainable recovery begins with deep, honest inquiry into the roots of behavior.


Related Post
The Next Big Shift After Erome Media: A Transformative Reckoning in Digital Content and Community Building

Miranda Harts Husband: Behind the Laughter – A Deep Dive into a Private Life Shaped by Public Fame

Toni Braxton’s Net Worth Hits $110 Million in 2022: A Resilient Music Legacy Valued at Over a Century in Data

Barbara 2233 Angel Number: Unlocking the Mystery of Twin Flame, Love, and Single Destiny

