Unlocking Early Stroke Diagnosis: How the Nih Stroke Scale Test Group A Answers Guide Critical Decisions
Unlocking Early Stroke Diagnosis: How the Nih Stroke Scale Test Group A Answers Guide Critical Decisions
In the race against time for stroke patients, precise assessment tools determine outcomes more than any treatment alone. The Nih Stroke Scale (NIH Stroke Scale), particularly when applied through the Group A answer patterns, serves as a frontline instrument for rapid stroke identification and severity classification. Trained clinicians rely on its structured evaluation to detect subtle neurological deficits within minutes—a capability proven to reduce critical delays in care delivery.
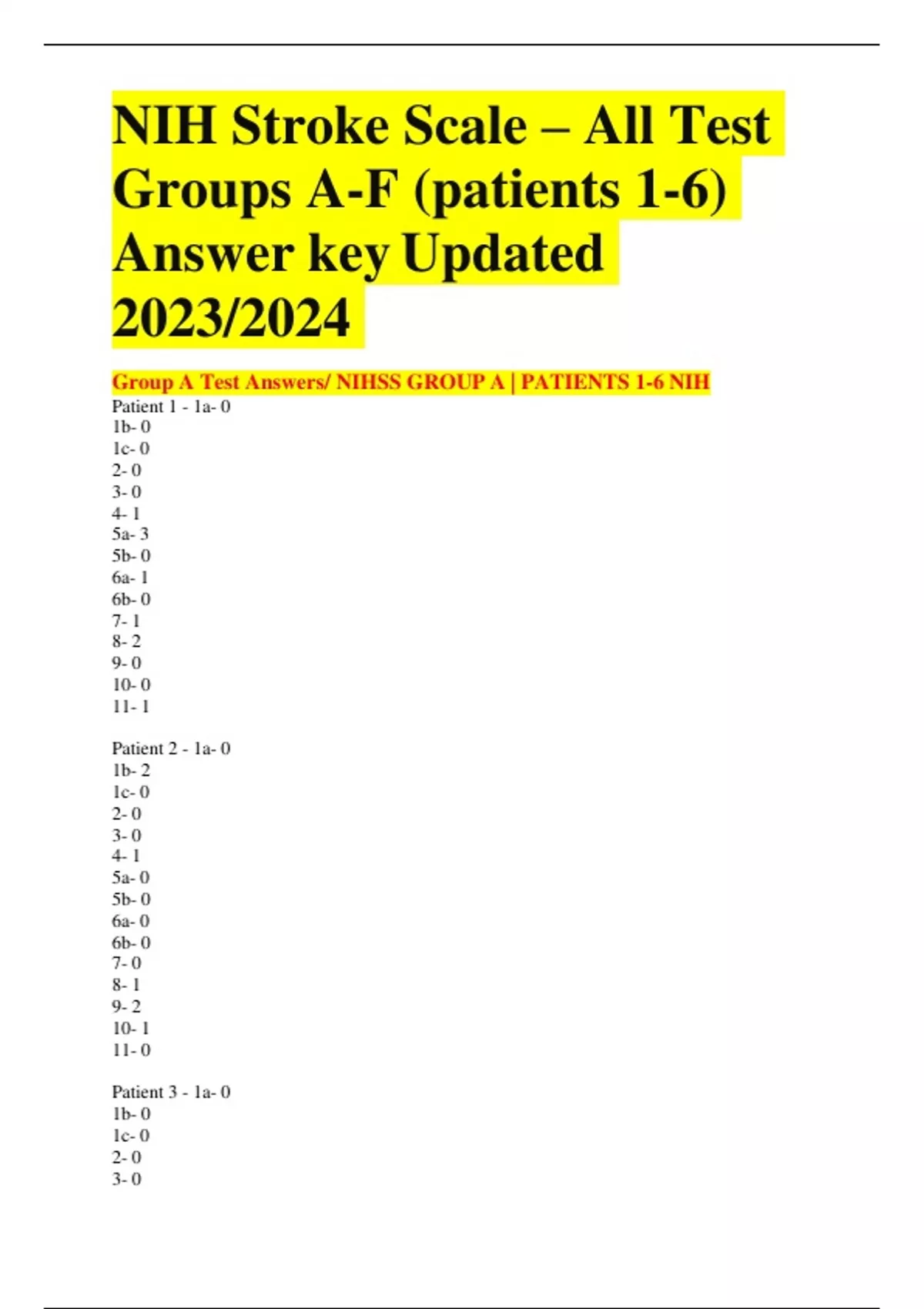
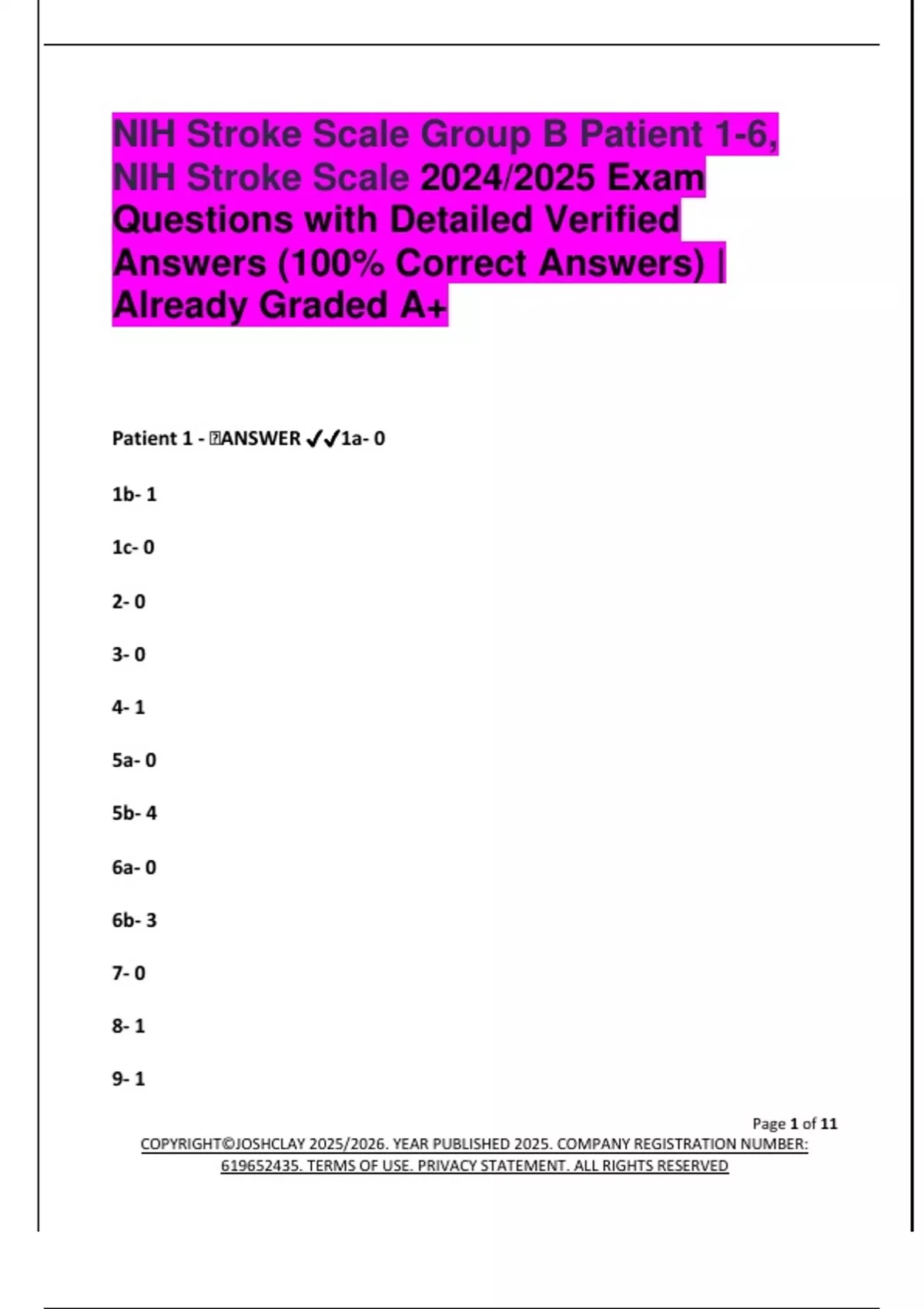
Understanding the Group A responses within the scale reveals not only progression risks but also guides real-time clinical interventions, transforming emergency response in acute stroke units globally. The NIH Stroke Scale is a standardized 15-item neurological assessment designed to quantify stroke effects across face, eyes, facial strength, speech, having trouble with words, arm and leg strength, sensory loss, and coordination. Each item consists of numerical scoring from 0 to 2, with higher totals indicating more severe impairment.
Of particular clinical urgency is Group A, which encompasses the most sensitive early indicators: facial droop, arm drift, and speech abnormality. These grouped responses often represent the first measurable signs, done within a typically 2–4 minute window during emergency triage.
Group A items are foundational to quick triage because they reflect core motor and cognitive functions immediately compromised in ischemic or hemorrhagic stroke.
The scale’s design prioritizes reproducibility without requiring advanced equipment, making it accessible across varied healthcare settings—from urban stroke centers to remote emergency departments. For Group A evaluations, each item demands meticulous observation: a suppressed facial expression, inability to extend arms evenly, slurred speech, or facial asymmetry each register as 0, 1, or 2 depending on severity. Experts emphasize that consistency in scoring prevents under-recognition, a common pitfall in high-pressure environments.
“A single missed motor deficit in Group A can delay thrombolytic therapy by critical minutes,” notes Dr. Elena Marquez, a neurologist specializing in acute cerebrovascular care. “The scale’s structured nature trains responders to identify these nuances systematically.” A typical Group A response pattern might include: - Facial drooping rated 1 or 2 due to incomplete eyelid closure or unilateral smile inability - Arm drift at 1 or 2 indicating weakness or paralysis on one side - Speech impairment rated 1 or 2, marked by slurring or word substitution - Oculomotor deficits observed during eye movement tests Each irrespectively low score collectively signals significant disruption—patterns validated by decades of stroke research and clinical practice.
The power of the NIH Stroke Scale Group A lies in its binary clarity: subtle deviations translate directly into measurable clinical urgency. For instance, a patient scoring 4 or more on Group A items typically triggers immediate imaging, notification of a stroke team, and initiation of potential clot-busting drugs. Clot removal procedures, effective within rigid time windows, depend entirely on frontline recognition—data from large trials like the EMERGENCY study confirm that every minute delays treatment and decreases recovery odds by 1–2%.
“We depend on Group A consistency to avoid false negatives under stress,” says Dr. Rajiv Patel, emergency medicine specialist. “A missed droop or slurred speech can mean the difference between full recovery and lasting disability.” Beyond speed, the NIH Scale Group A enables objective communication among emergency teams.
Standardized phrasing ensures that every responder—nurse, paramedic, or physician—uses the same language when describing deficits. This reduces ambiguity that often hampers timely coordination. For example, stating “患者在右侧显示明显面部不对称和右臂差力(2分)” (“Patient shows clear facial asymmetry and right arm weakness, 2 points”) provides a clear, actionable snapshot.
The scale’s numeracy—scores from 0 to 12—allows rapid risk stratification that aligns with national and international stroke guidelines, including those from the American Heart Association and World Stroke Organization.
Despite its simplicity, effective use of Group A responses demands focused training and vigilance. Studies reveal inter-rater variability when personnel lack structured practice; small nuances—such as partial arm drift or a barely noticeable facial falter—can be overlooked or overemphasized.
Therefore, ongoing education using the official NIH Stroke Scale training modules, including video demonstrations and real-time feedback, remains essential. “Standardization isn’t just about scoring—it’s about building muscle memory,” advises Nurse Linda Cho, a certified stroke nurse and NIH training coordinator. “When teams internalize Group A patterns, recognition becomes reflexive, cutting evaluation time while preserving accuracy.” Moreover, integration of the NIH Stroke Scale into digital health platforms enhances its real-world impact.
Electronic triage systems now auto-populate Group A scores, link to stroke hotlines, and trigger alerts in emergency routing protocols. In hybrid care models, where telemedicine supports pre-hospital stroke identification, Group A responses serve as objective data points that guide field treatment decisions. This synergy between clinical protocol and technology strengthens public health infrastructure, ensuring stroke recognition transcends geographic and resource limits.
practitioners emphasize that while advanced imaging and biomarkers continue to evolve, the NIH Stroke Scale—especially Group A—remains irreplaceable at the point of care. Its portability, cost-effectiveness, and proven reliability in diverse populations make it the cornerstone of global stroke readiness. Every parameter ruled within Group A answers is not merely data; it is a life-saving signal, a critical input that shapes treatment paths and ultimately, patient survival.
In summary, mastery of the NIH Stroke Scale Group A answers is indispensable for clinicians confronting acute stroke. Far from a routine check, this assessment is the frontline silent guardian—detecting early dysfunction, enabling rapid escalation, and anchoring evidence-based urgency. As stroke care advances, the scale’s enduring structure ensures that critical moments are not lost to uncertainty, reaffirming its status as an essential tool in neurology and emergency medicine.
The question now is not if this scale matters—but how consistently it is applied, measured, and trusted across every emergency setting where a stroke demands immediate mastery.



Related Post
Master Stroke Assessment: How the Nih Stroke Scale Group A Answers PDF Transforms Emergency Diagnoses

Blessed In The City: Fred Hammond’s Lyrics Reveal a Devotional Pulse to Urban Life