Unlock the Secrets of Male Reproduction: A Detailed Urutan Saluran Reproduksi Pria Labelled Diagram
Unlock the Secrets of Male Reproduction: A Detailed Urutan Saluran Reproduksi Pria Labelled Diagram
The human reproductive system in males is a marvel of biological precision, where a complex network of organs and physiological processes work in harmony to produce healthy gametes and enable fertility. Understanding the hierachy of male reproductive anatomy and function is essential for both medical professionals and individuals seeking clarity on how reproduction unfolds beneath the skin. By analyzing the Urutan Saluran Reproduksi Pria (male reproductive pathway), we uncover the sequential stages—from spermatogenesis to hormone regulation—that sustain life-giving functions.
This anatomical diagram serves not only as a visual education tool but as a scientific roadmap tracing how stimuli, hormones, and organs collaborate in perfect synchrony.
Step-by-Step Flow of the Urutan Saluran Reproduksi Pria
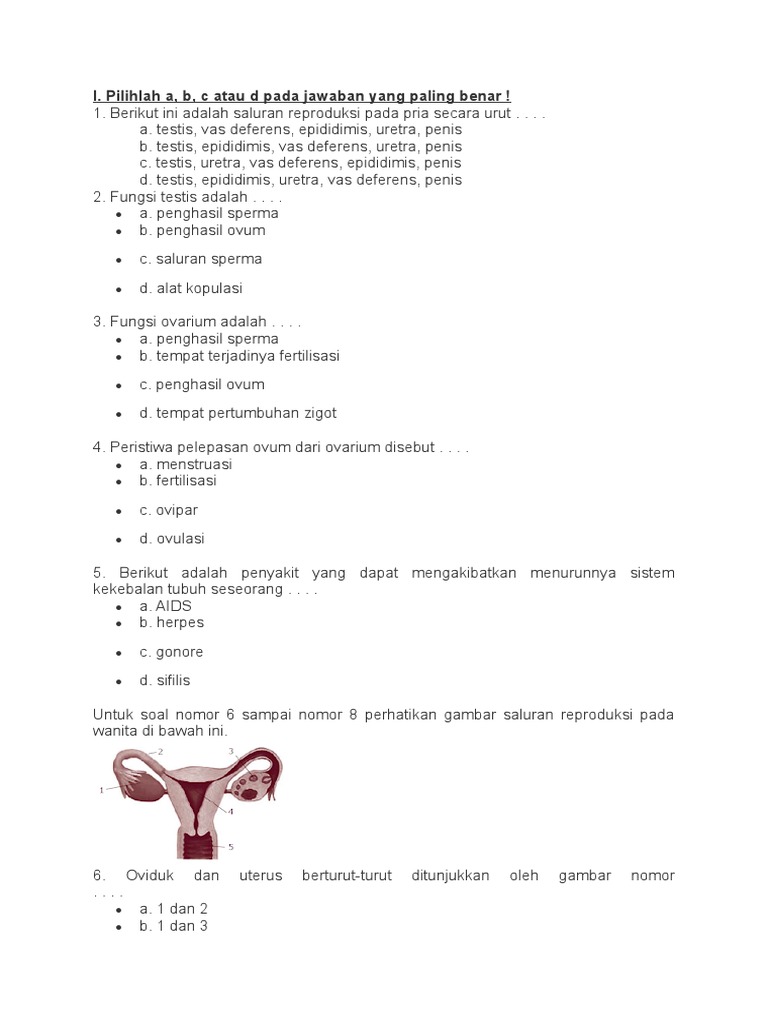
The reproductive journey in males is intricately coordinated: its etapas unfold in a precise sequence governed by endocrine signals and anatomical connections. Each phase is critical—disruption at any point can impact fertility or health. The full urutan saluran begins with the hypothalamus, proceeds through the pituitary, testes, and ductal system, and culminates in sperm release.
Below is a detailed breakdown of the process.
1. Hypothalamic Secretion of Gonadotropin-Releasing Hormone (GnRH)
The process initiates in the hypothalamus, a master regulator located deep in the brain. Under normal conditions, this region secretes Gonadotropin-Releasing Hormone (GnRH) in pulsatile bursts, triggering downstream activity critical for reproductive function.
“GnRH acts as the first switch in the male reproductive sequence,” notes Dr. Rahul Mehta, a reproductive endocrinologist. “Without this signal, the entire cascade stalls.”
2.
Anterior Pituitary Releases Follicle-Stimulating Hormone (FSH) and Luteinizing Hormone (LH)
GnRH stimulates the anterior pituitary gland to release two key hormones: Follicle-Stimulating Hormone (FSH) and Luteinizing Hormone (LH). Both hormones flow through the bloodstream to the testes, where they orchestrate intracellular activity essential for sperm production and testosterone synthesis. FSH specifically targets Sertoli cells within the testicular tubules, while LH acts primarily on Leydig cells.
3.
Sertoli Cells Enable Sperm Production through Spermatogenesis
Within the seminiferous tubules of the testes, Sertoli cells provide structural and nutritional support to developing sperm. Guided by FSH, these cells foster mitotic and meiotic divisions of spermatogonia—the stem cells responsible for sperm lineage. “Sertoli cells are the architects of sperm, building the microscopic scaffolding that allows each sperm cell to mature,” explains Dr.
Amara Okafor, a male reproductive specialist. This complex process—spermatogenesis—transforms undifferentiated germ cells into motile, mature spermatozoa, taking approximately 64 days from initiation to release.
4. Leydig Cells Produce Testosterone under LH Stimulation
As LH binds to Leydig cells on the outer testicular surface, it prompts them to synthesize and secrete testosterone—the primary male sex hormone.
Testosterone regulates not only sperm maturation but also the development of secondary sexual characteristics, libido, and overall reproductive health. “Testosterone is the biochemical engine driving male fertility and character,” emphasizes Dr. Okafor.
Circulating testosterone maintains the spermatogenic environment and supports libido and muscular development.
5. Hormonal Feedback Mechanisms Sustain Balance
To maintain equilibrium, testosterone and inhibin B—produced by Sertoli cells—are secreted into the bloodstream. These hormones feedback to both the pituitary and hypothalamus, dampening GnRH, FSH, and LH release in a delicate negative feedback loop.
“This feedback system ensures hormone levels remain stable,” says Dr. Mehta. “Any imbalance—such as low testosterone—can reduce FSH and LH, ultimately impairing sperm production.”
6.
Sperm Maturation and Transport Through Accessory Ducts
Mature sperm exit the seminiferous tubules and enter a network of ducts: the rete testis, efferent ductules, epididymis, and vas deferens. The epididymis is pivotal—here, sperm undergo functional maturation, gaining motility and the ability to fertilize an egg. “It’s within the epididymis that sperm transform from relatively immotile cells into dynamic, capable entities ready for ejaculation,” notes Dr.
Mehta. From there, contractions during ejaculation propel sperm through the vas deferens and into the urethra.
7. Ejaculation and Release of Spermatogenesis Products
Marked by coordinated contractions during sexual arousal, ejaculation delivers sperm-laden seminal fluid into the urethra.
This final step is not merely expulsion; it is the culmination of hours of hormonal signaling, cellular development, and physiological preparation. Once released, sperm are equipped—harnessed by years of biological programming—to fulfill their purpose: fertilization.
The Urutan Saluran Reproduksi Pria is far more than a diagram—it is a timeline of biology in motion. Every organ, hormone, and signal plays a non-negotiable role, reflecting millions of years of evolutionary refinement.
Understanding this chain enables early detection of reproductive disorders, supports advancements in assisted reproductive technologies, and empowers informed decisions about gender health. As medical science continues to decode the subtleties of male fertility, this visual roadmap remains indispensable—blending education, precision, and practical insight for anyone seeking to understand how life begins within


Related Post
Sonya Deville and Toni Cassano Exchange Vows in Heartwarming Ceremony
Discovering MovieHD: Your Ultimate Guide to Streaming Movies Online

How Tall Is Playboi Carti? The Precise Stature Behind the artistes

Picnic Restaurant Jackson Wy Redefines Outdoor Dining in a Jackson County Gem

