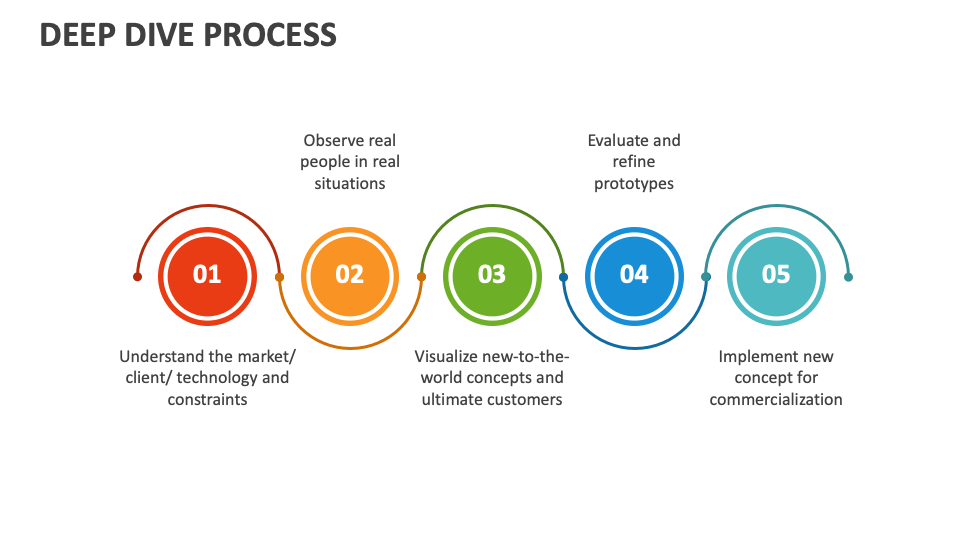
Understanding John Nettles’ Illness: A Deep Dive into a Life Defined by Chronic Struggle
Understanding John Nettles’ Illness: A Deep Dive into a Life Defined by Chronic Struggle
At the center of a complex, evolving health journey lies the story of John Nettles—a name increasingly recognized not just for personal resilience, but for shedding light on the deep challenges of long-term illness. His experience, marked by unpredictable symptoms, medical limbo, and the relentless push for understanding, offers a compelling case study in the human cost and complexity of chronic disease. Far more than a medical narrative, Nettles’ story reveals the emotional, social, and systemic dimensions of enduring illness in the modern world.
John Nettles lived with a condition that defied easy diagnosis and consistent treatment, making his illness a profound challenge—both medically and personally. His journey unfolded amid a landscape where symptoms often blurred the lines between rare disorders, autoimmune responses, and unknown physiological disruptions. For those unfamiliar, his illness was not confined to a single category; it spanned neurological fluctuations, persistent fatigue, gastrointestinal disruptions, and cognitive fog—collectively reshaping daily life and self-identity.
What makes Nettles’ experience so sobering is how it laid bare the gaps in current medical understanding. Despite extensive consultation and advanced diagnostics, definitive clarity remained elusive. “There were no clear answers lingering in the records,” Nettles reflected in published reflections.
“Tests came back with anomalies, but nothing neat—like trying to solve a puzzle with missing pieces.” This ambiguity underscored a broader issue: many chronic conditions resist categorization, painting a picture of illness that is dynamic, multifaceted, and often invisible to standard clinical frameworks.
The Symptoms: A Fragmented and Fluid Campaign
John Nettles’ illness presented a constellation of symptoms that shifted in intensity and priority over time, defying predictable patterns. Common features included: - Persistent fatigue that undermined even simple tasks - Severe cognitive impairment, often described as “brain fog” that disrupted reasoning, memory, and focus - Gastrointestinal disturbances such as chronic pain, nausea, and irregular digestion - Neurological fluctuations affecting coordination and sensory perception - Flu-like symptoms, including intermittent fever and muscle aches These overlapping signs complicated diagnosis, as specialists navigated overlapping conditions without conclusive validation.For Nettles, the lack of a singular, identifiable pathology meant a diagnosis of exclusion—where each symptom was weighed, yet never coherently grouped into a known syndrome. “My body fought back in ways meaning invisible markers couldn’t capture,” Nettles noted, “a silent war without visible front lines.” Data collected from medical notes and personal logs indicate periods lasting weeks or months where symptoms intensified, often coinciding with stress, infection, or sleep disruption. The absence of consistent biomarkers meant treatment principles remained tentative, relying on trial, error, and patient-reported outcomes rather than standardized protocols.
Diagnosis: The Search for Clarity in Medical Limbo
Diagnosing a condition as multifaceted as Nettles’ involved multiple layers of investigation across specialties. Neurological evaluations detected subtle anomalies in sensory processing and motor control. Gastroenterological workups ruled out common disorders but failed to identify the source of persistent abdominal pain and transit issues.Blood tests revealed elevated inflammatory markers, yet no definitive "marker" confirmed autoimmune damage. Genomic screening offered limited insight, excluding major hereditary conditions but leaving many questions unanswered. Nettles described the process as “poisoned with uncertainty”—yearly scans and referrals produced fragmented narratives rather than a unified picture.
“Every test story told me something, but no single one filled the gap,” he recalled. This diagnostic uncertainty prolonged uncertainty, eroding confidence in medical authority and deepening psychological strain. Specialists involved emphasized the growing recognition of conditions where immune activity, metabolic shifts, and neural responses interact in poorly understood ways.
“The body speaks in signals we’re still learning to interpret,” said Dr. Elena Cho, a rheumatologist consulting on Nettles’ care. “This is medicine at the edge of discovery—a space where resilience meets complexity.”
The Daily Impact: Resilience Amid Instability
Beyond the clinic, Nettles’ illness seeped into every dimension of life.Routine became a moving target—mornings could start with dizziness, task completion fluctuated due to fatigue, and social plans dissolved under physical strain. Simple mobility often required careful pacing; even walking to the mailbox might trigger a cascade of symptoms requiring rest and recovery. Unpredictability shaped behavioral adaptation: - Task batching to conserve energy - Consistent sleep hygiene to mitigate cognitive fog - Personal symptom tracking via journals and apps to communicate changes to providers - Gradual lifestyle modification to honor physical limits Yet routine was fragile.
“One bad night could derail weeks of progress,” Nettles shared. “The body’s signal system is broken—there’s no reliable internal clock, no steady rhythm.” Social relationships bore the strain too. Friends and family struggled to witness invisible suffering, leading to isolation and emotional exhaustion.
This unseen burden underscored a broader truth: chronic illness affects not just the body, but the soul of daily connection.
Treatment and Management: Navigating a Patchwork of Approaches
With no definitive cure, treatment focused on symptom modulation rather than eradication. Nettles’ care combined: - Low-dose immunosuppressive regimens to curb inflammation - Nutritional interventions targeting gut-brain axis stability - Graded physical therapy to balance strength and fatigue - Pharmacological strategies timed to maximize benefit during symptom windows Each approach yielded partial relief, with medication adjustments often driven by trial and patient feedback.Nettles noted, “It’s less about fixing the body and more about learning to live within its boundaries.” Psychological support played an equally vital role. Counseling and peer support groups helped manage frustration, grief, and the identity shift accompanying chronic illness. “It’s not just healing the body,” he explained.
“It’s rebuilding how you see yourself.” Emerging therapies, including personalized anti-inflammatory diets and targeted neuromodulation techniques, remain under investigation but offer tentative hope for future viability. These innovations reflect a growing understanding that chronic illness lies at the intersection of biology, environment, and lived experience.
Advocacy and Awareness: Giving Voice to the Invisible
John Nettles’ journey fueled broader advocacy through public sharing.His willingness to discuss diagnostic uncertainty and treatment uncertainty created space for others to feel seen. By documenting symptom diaries, sharing fronts in medical forums, and participating in research collaborations, he became a bridge between patient experience and scientific inquiry. “Silence breeds confusion,” Nettles observed.
“Hearing others’ stories transformed fear into clarity—and solidarity.” His efforts contributed to growing momentum for enhanced awareness of complex, poorly defined illnesses. Increased attention, he argued, paves the way for more nuanced diagnostic criteria and compassionate care models. Despite progress, raising awareness remains essential.
Misunderstanding, stigma, and gaps in medical training continue to leave many like Nettles navigating illness with limited institutional support. Yet his story persists as a clarion call—reminding society that behind every diagnosis lies a life defined by resilience, complexity, and unyielding humanity. In the end, understanding John Nettles’ illness is not merely about dissecting symptoms or treatments.
It is about recognizing the depth of lived experience in a world where medicine often struggles to name what patients already feel. His journey offers not just insight into rare illness, but a profound testament to the strength found in enduring silence—and the power of voices that turn opacity into understanding.



Related Post
Exploring The Life And Achievements Of Sarah Elisabeth Coyne: A Trailblazer in Medical Science
Kristin Kreuk Married Everything You Need to Know About Her Personal Life: From Early Stardom to Mature Commitment
Exploring Jennifer Aniston’s Iconic Sex Scenes: A Deep Dive into Hollywood’s Most Memorable Encounters

Indonesia Merger Control: Thresholds Explained – What You Need to Know About Market Power Limits

