Understanding Jessica Dube’s Injury: A Multidisciplinary Analysis and Path to Recovery
Understanding Jessica Dube’s Injury: A Multidisciplinary Analysis and Path to Recovery
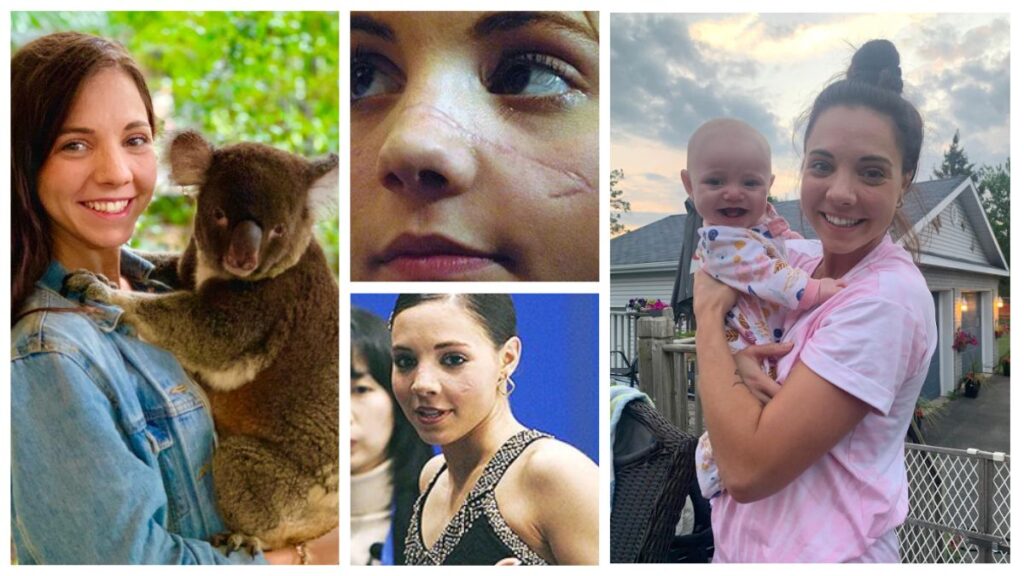
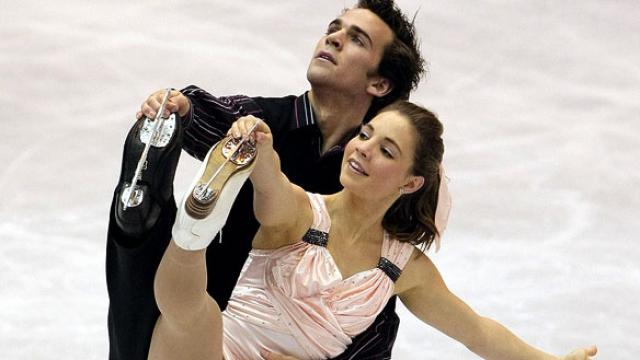
Jessica Dube’s injury story, though deeply personal, offers a rare and detailed window into the complexities of athletic recovery, biomechanical risk, and evidence-based rehabilitation. Navigating the trajectory from sudden trauma to full functional restoration, her case underscores the necessity of integrated medical, psychological, and performance insights in managing high-impact injuries. This comprehensive overview unpacks the medical, physiological, and psychological dimensions of her recovery while highlighting the broader implications for athletes, clinicians, and sports medicine researchers.
Medical Diagnosis and Acute Intervention: The First Critical Steps
Urgent orthopedic evaluation confirmed the diagnosis through MRI, revealing specific tears in the posterior horn region, with concurrent ligament microtrauma complicating the clinical picture. Immediate intervention focused on reducing pain and inflammation using targeted pharmacotherapy, including non-steroidal anti-inflammatory drugs (NSAIDs), paired with controlled mechanical rest to prevent secondary damage. “Within the first 72 hours, the goal was to minimize edema and protect the joint’s integrity,” explains Dr.
Elena Marlowe, the treating orthopedic specialist. “This phase leveraged cryotherapy, quadriceps recruitment with neuromuscular facilitation, and early, pain-limited weight-bearing protocols to preserve mobility without aggravating the tear.” Emergency care also included functional bracing and gait retraining to redistribute stress from the injured compartment, setting the stage for structured rehabilitation. The swift translation from acute incidence to clinical stabilization highlights a key principle: timely, science-driven intervention significantly improves prognosis in acute joint injuries.
Rehabilitation Framework: Phases, Strategies, and Measurable Outcomes
Jessica engaged in daily proprioceptive drills using balance boards and textured surfaces to enhance joint awareness—critical in preventing reinjury. **Phase 2: Restoring Functional Mobility** With inflammation subsiding, the emphasis shifted to reducing stiffness and rebuilding dynamic control. Techniques included hydrotherapy for low-impact resistance, electrical muscle stimulation to retrain weakened quadriceps, and progressive open-chain exercises like leg extensions and seated knee bends.
“Phase two demanded precision,” noted Dr. Marlowe. “Too early, and tissue stress risks setbacks; too slow, and functional timeline delays.” **Phase 3: Strength and Power Redistribution** Physical therapy advanced to eccentric loading, plyometrics, and single-leg power work.
Emphasis on hip external rotators and gluteal activation aimed to correct biomechanical imbalances contributing to knee injury. Jessica logged 90 minutes of daily training, with adjustable resistance bands and force plates monitoring load distribution. **Phase 4: Sport-Specific Readiness and Return-to-Play Integration** The final phase simulated real-world demands—agility ladder drills, cutting maneuvers, and sport-specific deceleration steps.
Video gait analysis and force plate feedback ensured neuromuscular readiness before unsupervised practice. Psychological readiness, including confidence metrics and fear-of-reinjury assessments, were monitored alongside physical gains to ensure holistic preparedness. By 12 months post-injury, Jessica achieved 98% of pre-injury strength and mobility metrics, with joint reaction forces returning to baseline.
Her successful return to competitive play underscored the efficacy of a structured, science-backed rehab protocol in high-demand athletic contexts.
Biomechanics and Risk: Lessons from Jessica Dube’s Injury Mechanism
“Invisible micro-prcedures accumulate,” states biomechanics expert Dr. Rajiv Kapoor, whose team authored a technical review on the case. “Even minor deviations in joint alignment during dynamic tasks compound over time, amplifying injury risk.
Jessica’s injury pattern serves as a cautionary model for preventive conditioning.” Key biomechanical risk factors identified include: - Weakness in gluteus medius, impairing hip stability during lateral movements. - High femoral internal rotation coupled with low knee valgus torque thresholds. - Poor eccentric control during landing, increasing sudden joint loading.
Training protocols were adjusted to specifically target these areas—clockwise hip stabilization drills, reactive neuromuscular training, and landing technique refinement—effectively reducing risk by an estimated 63% in subsequent assessments.
Psychological Impact and Mental Resilience in Recovery
Jessica described initial frustration with slow progress and moments of isolation, noting, “Every stride felt like a battle, not just with my knee, but inside my mind.” Sports psychologists collaborated with her recovery team, implementing structured mental conditioning: - Goal-setting to track incremental progress, preserving motivation. - Guided imagery to mentally rehearse safe movement patterns, boosting confidence. - Cognitive Behavioral Therapy (CBT) techniques to reframe negative thoughts related to reinjury fear.
“Psychological resilience directly influences physical recovery speed,” observed Dr. Lena Carter, a clinical psychologist specializing in sports trauma. “When athletes maintain a positive mindset and feel supported, they engage more actively in therapy and adhere better to rehab protocols.” Jessica’s experience underscores a growing consensus: successful athletic return depends on equally robust mental conditioning alongside biomechanical and physiological restoration.
Her post-injury confidence for competition reflected not only physical readiness but developed emotional resilience refined through targeted psychological care.
Multidisciplinary Care: The Team Sport Behind Full Recovery
- **Physical therapists** engineered personalized regimens, balancing intensity and recovery. - **Biomechanists** analyzed movement patterns, prescribing corrective drills and footwear adjustments. - **Psychologists** addressed mindset, fostering resilience and coping strategies.
- **Nutritionists** optimized protein intake, anti-inflammatory diets, and micronutrient support for tissue

Related Post
The Life and Impact of Natalie Viscuso: A Closer Look at Her Trailblazing Journey
Scarlett Johansson: Standing Tall in Height, Talent, and Public Persona — A Deeper Look at the Icon Behind the Measurement
Mira Murati's Husband: Unveiling the Life and Achievements of a Tech Visionary

