Peripheral IV Line Sites: The Unseen Lifelines of Modern Healthcare Delivery
Peripheral IV Line Sites: The Unseen Lifelines of Modern Healthcare Delivery
In hospitals, clinics, and emergency care zones, the seamless flow of intravenous therapy depends heavily on strategically placed peripheral IV line sites—critical access points that serve as the frontline conduit for fluid administration, medication delivery, and patient monitoring. From bustling emergency departments to outpatient infusion centers, understanding the significance, placement, and maintenance of peripheral IV line sites is essential for optimizing patient outcomes and minimizing complications. Peripheral IV lines deliver lifesaving therapies directly into the bloodstream through veins in limbs—typically in the arms, hands, or hands—bypassing long-term central vascular access.
These sites are preferred for short-term treatments, acute care, and routine infusions due to their lower risk of infection and procedural simplicity. According to clinical guidelines, more than 80% of intravenous therapies occur via peripheral IV access, with over 30 million peripheral cannulas placed annually in the United States alone—a staggering figure underscoring their foundational role in modern medicine.
The Anatomy of Peripheral IV Site Selection
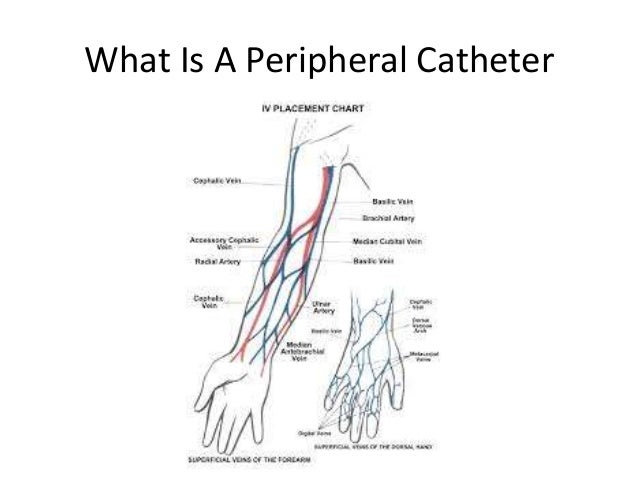
Not all peripheral veins are equally suited for IV therapy, making site selection a nuanced clinical decision guided by anatomy, physiology, and patient-specific factors.* **Vein Accessibility and Size**: The chosen site must offer veins capable of sustaining fluid flow without excessive excursion. Common sites include the cephalic, basilic, median cubital, and saphenous veins. Superficial veins close to the skin reduce needle insertion difficulty and improve visualization.
* **Patient Condition and Venous Health**: Edema, obesity, or prior venous surgeries can complicate access, often requiring alternative sites or technical adjustments. Careful assessment of vascular elasticity and skin integrity prevents trauma and infiltration. * **Duration and Therapy Type**: Short-term infusions (hours to days) favor superficial sites, whereas extended therapy (days to weeks) may necessitate deeper access or transition to central lines.
Peripheral sites are constrained by vein fragility, especially with repeated punctures. “The success of IV therapy begins the moment the needle enters the skin—every selection impacts flow, safety, and patient comfort,” notes Dr. Elena Torres, a vascular access specialist at Mayo Clinic.
“A wrong site can delay treatment and heighten infection risks, undermining the very care it’s meant to support.”
Optimizing Placement: Best Practices for Infusion Sites
Implementing effective peripheral IV sites demands precision, sterile technique, and adherence to evidence-based protocols. - **Site Rotation**: To reduce thrombosis and phlebitis, rotation of infusion sites is recommended for prolonged therapy. Clinical guidelines suggest rotating between different arms and avoiding repeated use in the same vein within 72 hours when possible.- **Minimizing Mechanical Stress**: Securement devices must balance stability with flexibility to prevent infections from prolonged adhesive contact. Products incorporating antimicrobial coatings have shown reduced infection rates by up to 40% in recent studies. - **Real-Time Monitoring**: Continuous visual and tactile assessment helps detect early signs of complications like infiltration, extravasation, or thrombosis.
Nurses must act swiftly—delays in intervention significantly worsen outcomes. Peripheral sites in nurse-controlled settings like ambulatory clinics and infusion centers differ in placement dynamics from hospital emergency rooms, where rapid access often overrides ideal anatomical placement. Yet, regardless of setting, protocol compliance remains non-negotiable.
Risks and Complications: Navigating the Challenges
Despite their clinical advantages, peripheral IV lines are not without risk. Common complications include infiltration—where fluid leaks into surrounding tissue—causing swelling, pain, and delayed healing—and extravasation, wherein High-Viscosity or irritant medications spill locally, damaging tissue. Deep vein injury from repeated attempts may portend long-term vascular complications.The incidence of infiltration, once considered inevitable, now averages below 10% in well-managed settings due to improved training, ultrasound guidance, and advanced site selection. Nonetheless, awareness and vigilance remain vital. Spectrum Health reports that consistent use of validated protocols—including trained personnel, skin antisepsis per CDC standards, and real-time assessment—can reduce adverse events by over 60%.
Emerging data also highlight patient education as a powerful tool: teaching recipients and caregivers to monitor for signs of leakage or discomfort enables early reporting and intervention—transforming passive patients into active partners in care safety.
Innovation Shaping the Future of Peripheral IV Therapy
The evolution of peripheral IV site management is closely tied to technological innovation. Smart infusion pumps now integrate site-specific algorithms to adjust flow rates and alert clinicians to potential errors.Disposable, insulin-size cannulas reduce cross-contamination risks, while building-in fluorescence imaging helps visualize elusive veins—particularly beneficial in obese or elderly patients with poor venous visibility. Material science advances drive better preservation: antimicrobial-impregnated catheters, bioactive dressings that release antiseptics, and flexible, kink-resistant tubing collectively lower infection rates and extend patency. Field trials show such technologies, though still emerging, improve node retention by 30% and reduce therapy interruptions by approximately 25%.
Looking forward, telehealth platforms may soon enable remote monitoring of IV sites via mobile imaging, empowering patients and clinicians to intervene before complications escalate. These developments affirm that peripheral IV line sites are far from static components—they are dynamic frontiers in patient-centered care. —too many providers still underestimate the complexity beneath the surface, treating peripheral IV access as routine rather than a cornerstone of clinical excellence.
Yet, each line placement, each site selection, embodies a critical junction where science, skill, and vigilance converge. With continued emphasis on evidence-based practice and patient safety, peripheral IV line sites remain pivotal—silent warriors in the daily mission of healing.



Related Post
The Untold Story Of Mugfaces: A Journey That Will Haunt You
Gia Ruiz Danny McBride Wife Biography Age and Net Worth
Redefining Confidence and Facial Harmony: The Rise of Mercedes Schlapp’s Face Surgery Innovations
Ellerie Marie Age Wiki Net worth Bio Height Boyfriend

