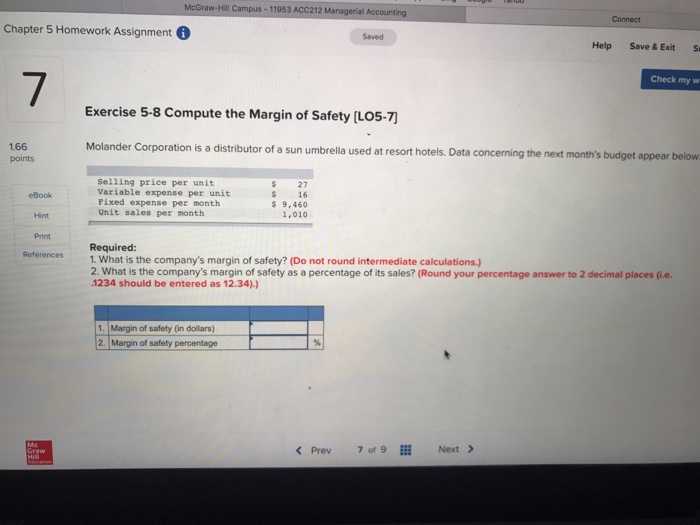
Mastering Blood in Human Physiology: Key Insights from McGraw Hill’s Chapter 10 Answers;
Mastering Blood in Human Physiology: Key Insights from McGraw Hill’s Chapter 10 Answers;
Blood is the body’s dynamic transportation network, responsible for delivering oxygen, nutrients, hormones, and immune defenders while removing waste—making it central to human survival. According to McGraw Hill Human Anatomy and Physiology Chapter 10, understanding blood involves dissecting its complex cellular composition, functional roles, regulatory mechanisms, and clinical significance. From red and white blood cells to clotting factors and the circulatory system’s intricate coordination, this chapter reveals the sophisticated biology behind blood’s life-sustaining duties—and why its disruption underlies countless diseases.
The Cellular Architecture of Blood: Red, White, Platelets, and Plasma
Blood’s functional capacity stems from four primary cellular components, each fulfilling specialized roles.
Red blood cells (erythrocytes) are nucleated, biconcave marvels designed to maximize oxygen transport—each cell carries about 270 million hemoglobin molecules, enabling a single red blood cell to deliver roughly 250 million molecules of oxygen in a minute. White blood cells (leukocytes) form a vital arm of the immune system, classified into granulocytes (neutrophils, eosinophils, basophils) and agranulocytes (lymphocytes, monocytes), each targeting different pathogens through phagocytosis, antibody production, or alert signaling. Platelets, or thrombocytes—small cell fragments—play a crucial role in hemostasis, adhering to damaged vessel walls and orchestrating clot formation.
Plasma, the liquid matrix, carries nutrients, hormones, clotting factors, and waste, composing about 55% of total blood volume. This distributed circuit ensures systemic coordination, a system “engineered” for peak efficiency.
Each cell type’s morphology and function reflect millions of years of evolutionary refinement. Erythrocytes, devoid of nuclei, achieve remarkable flexibility to squeeze through capillaries just 5–8 micrometers wide.
Neutrophils, the most abundant white blood cells, respond within minutes to infection, deploying neutrophil elastase and reactive oxygen species to neutralize bacteria. Platelets aggregate rapidly at injury sites, forming plugs stabilized by fibrin networks—a balance vital to prevent excessive bleeding or dangerous clots.
Oxygen, Carbon Dioxide, and the Gas Exchange Pipeline
The circulatory system’s primary physiological mandate is gas transport, managed primarily by red blood cells. Hemoglobin binding oxygen in the oxygen-rich lungs forms oxyhemoglobin, which delivers O2 to tissues where partial pressure gradients prompt release.
Simultaneously, carbon dioxide—byproduct of cellular respiration—is carried back to the lungs for exhalation. Unlike oxygen, CO2 moves via simpler diffusion, dissolving directly in plasma (~7%) and binding to hemoglobin (~23%), along with bicarbonate ions (括制) formed through CO2 hydration catalyzed by carbonic anhydrase. This biochemical pathway ensures efficient removal of metabolic waste without relying on dedicated “CO2 cells.”
Clinical studies cited in Chapter 10 emphasize the precision of this gas exchange.
Disruptions—such as impaired hemoglobin affinity in cyanide poisoning or reduced diffusion in emphysema—demonstrate how delicate oxygen delivery balance is. Moreover, blood pH is tightly regulated through bicarbonate buffering, a mechanism that prevents acidosis or alkalosis, maintaining optimal enzyme function across tissues.
Blood Clotting: A Chaotic Yet Regulated Cascade
When vascular injury occurs, hemostasis initiates a tightly regulated cascade to stop bleeding—partially governed by platelets and partially by the coagulation cascade. Platelets adhere to exposed collagen via von Willebrand factor, activating and aggregating into a temporary plug reinforced by fibrin strands from thrombin-generated fibrin.
The cascade involves 12 sequential clotting factors, initiated by tissue damage and exquisitely sensitive to imbalances—explaining why inherited disorders like hemophilia or acquired risks such as warfarin use dramatically increase bleeding tendency.
Chapter 10 underscores that clotting is not merely a mechanical seal but a biochemical symphony. Thrombin, a serine protease central to this process, activates platelets and converts fibrinogen to fibrin, while natural anticoagulants like antithrombin III and protein C prevent overclotting. This dual check—rapid response coupled with controlled termination—avoids thrombosis, a leading cause of myocardial infarction and stroke.
Blood Volume, Cellular Ratios, and Clinical Implications
Total blood volume averages 7–8% of body weight, differing by sex and size—men typically have higher volumes due to greater mass and muscle mass.
This balance is critical: reductions signal hemorrhage or anemia, while excess volume impairs cardiovascular efficiency. Red blood cell count and hemoglobin concentrations directly influence oxygen-carrying capacity, a parameter measured via complete blood counts (CBC) to diagnose conditions like iron deficiency anemia or polycythemia vera.
Disorders in blood physiology span from surplus—such as polycythemia—and deficit, to dysfunctions like sickle cell anemia or hemophilia. Each reveals the interdependence of blood’s components; dysfunction in one part cascades systemically.
For example, thrombocytopenia increases hemorrhagic risk, impairing wound healing and elevating stroke risk—directly illustrating blood’s role beyond circulation, as a central regulator of survival.
The Integration of Structure and Function: A Systemic Symphony
McGraw Hill’s Chapter 10 crystallizes blood not as a static fluid but as a dynamic, adaptive system where structure defines function and function shapes physiology. From hemoglobin’s oxygen binding to platelet-driven clotting across microcirculations, each mechanism is a testament to evolutionary precision. Understanding these processes is vital for clinicians managing hemorrhage, thrombosis, and hematologic diseases, reinforcing blood’s status as a cornerstone of human health—one that demands mastery for both science and medicine.
Blood’s centrality in physiology makes it indispensable to life, and Chapter 10 offers a lens through which its complexity is both accessible and profoundly relevant.
Grasping these principles transforms abstract anatomy into actionable knowledge—each insight a step toward diagnosing, treating, and ultimately preserving life itself.



Related Post

What Jobs Involve Trigonometry: The Unsung Mathematical Force Behind Key Professional Roles
Skor Langsung Basket: Indonesia’s Grit Against China in Elite World Basketball Showdown

