Keratinized Oral Mucosa: The Body’s Durable Oral Shield
Keratinized Oral Mucosa: The Body’s Durable Oral Shield
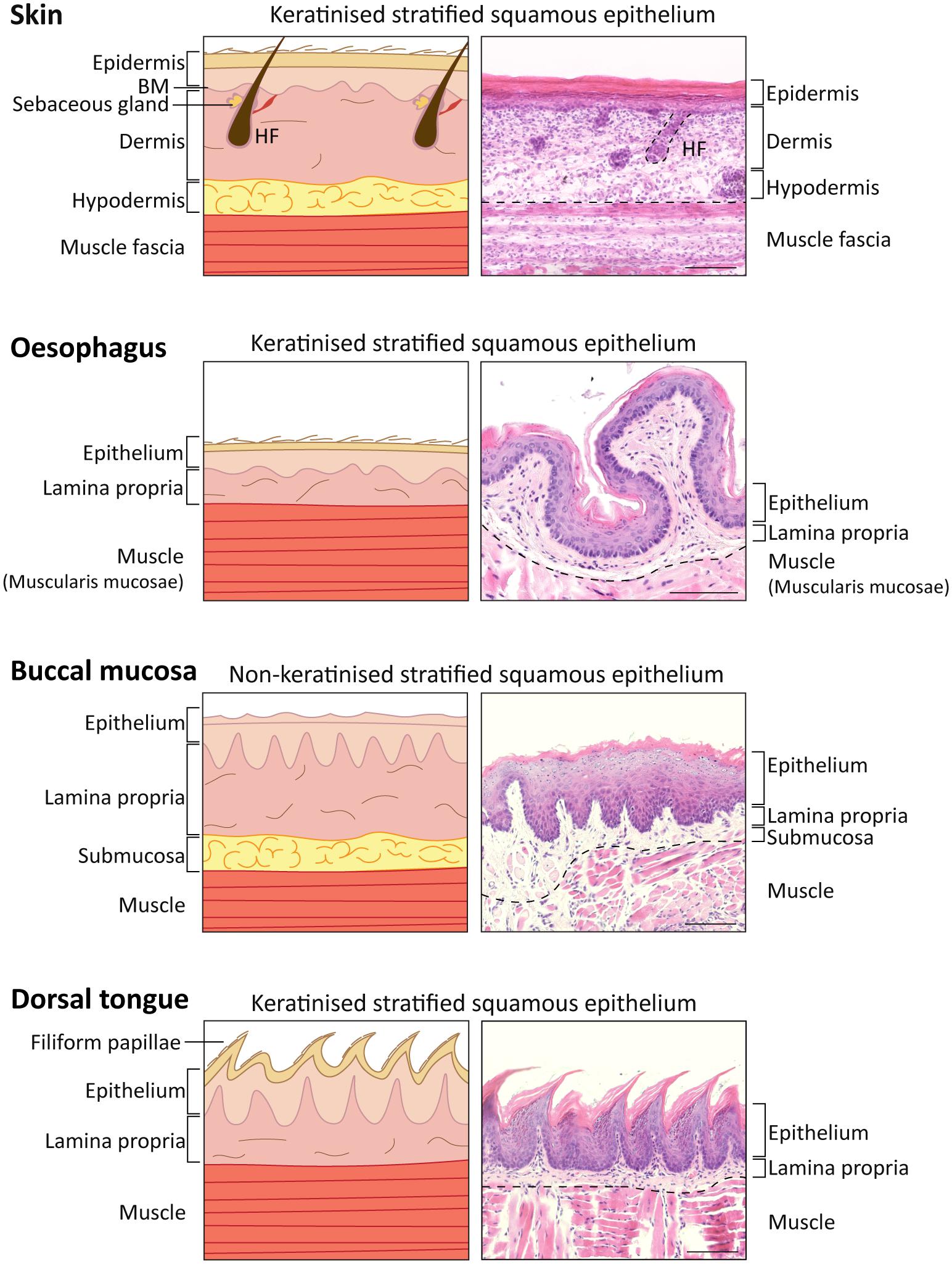
The keratinized oral mucosa, a specialized layer lining the inner cheeks, floor of the mouth, and gingival margins, serves as a critical biological barrier that protects underlying tissues from mechanical stress, microbial invasion, and chemical exposure. Unlike its non-keratinized counterparts in the palate or soft palate, this keratinized stratified squamous epithelium undergoes pronounced keratinization, endowing it with extraordinary resilience—an evolutionary adaptation to the constant friction, moisture, and microbial challenges of daily oral function.
Structurally, keratinized oral mucosa is distinguished by its dense arrangement of keratin filaments interwoven within tightly packed epithelial layers.
This keratinization process, driven by keratinocyte differentiation, transforms living cells into hardened, protective shields. Each superficial stratum contains fully keratinized cells, creating a continuous armor resistant to abrasion from chewing, speech, and food, as well as exposure to enzymes, acids, and pathogens. Clinically, this structural robustness not only preserves tissue integrity but also plays a pivotal role in maintaining mucosal health and preventing ulceration.
Biological Function and Adaptive Significance
The primary role of keratinized oral mucosa lies in defense and protection.As the first line of defense in the oral cavity, it shields delicate underlying structures—including blood vessels, nerves, and connective tissue—from daily wear and tear. The presence of keratin prevents excessive water loss and undergoes regulated turnover, balancing durability with cellular renewal. “This balance between hardness and regenerative capacity ensures that the mucosa remains functional without compromising flexibility,” explains Dr.
Elena Ramirez, a mucosal pathologist at the University of Barcelona’s Institute of Oral Biology. Beyond physical protection, the keratinized layer also modulates microbial interactions. Although not as dense as the epithelial barrier in the digestive tract, its surface aids in controlling microbial colonization by resisting microbial penetration and facilitating clearance through natural tissue turnover.
Research published in Oral Diseases highlights that keratinized mucosa “exerts selective permeability,” allowing essential immune surveillance while blocking invasive pathogens.
Clinical Relevance and Oral Health Implications
Understanding keratinized oral mucosa is essential for clinicians diagnosing oral pathologies and managing mucosal disorders. Areas with keratinization—such as the gingival margin and labial mucosa—are less prone to superficial fissuring, aphthous ulcers, and mechanical abrasion compared to non-keratinized regions. This explains why smokers, who often experience mucosal thinning, face higher risks of ulceration and delay healing in keratin-deficient zones.Conditions like lichen planus and pemphigoid frequently target keratinized tissues, prompting researchers to explore how structural integrity influences disease progression and treatment outcomes. “Preserved keratinization correlates with better mucosal resilience—patients with intact keratinized layers typically experience faster recovery and reduced symptomatic visits,” notes Dr. Raj Patel, a oral medicine specialist at Johns Hopkins.
Furthermore, the keratinization status serves as a vital diagnostic marker. Biopsy evaluation routinely assesses keratin layer thickness to differentiate benign lesions from premalignant conditions. “A reduction or irregular keratinization may signal chronic irritation or underlying systemic disease,” explains Dr.
Lin Zhang, a pathologist at Harvard-affiliated Brigham and Women’s Hospital.
Developmental and Variability Patterns
The distribution of keratinized oral mucosa follows distinct anatomical patterns influenced by biomechanical stress and mucosal function. The hard palate and gingival margins exhibit thick keratinized epithelium, while the inner cheeks and floor of the mouth house regions with thinner, non-keratinized tissue optimized for flexibility.This variability reflects evolutionary adaptation: high-friction zones require enhanced protection, whereas areas involved in dynamic movement benefit from tissue elasticity. Congenital variations exist, such as in patients with mucocutaneous lupus or genetic keratinization disorders, where abnormal keratinization leads to fragile, ulcerated mucosa. Pediatric mucosal development also shows progressive maturation—keratinization increases gradually from infancy through adolescence, reaching full maturity in adulthood.
Impact of Lifestyle and Environmental Factors
Lifestyle and environmental exposures significantly influence keratinized oral mucosa health. Tobacco use remains one of the most detrimental—inhibiting normal keratinocyte turnover and reducing mechanical durability. Chronic alkaline exposure from certain foods or oral hygiene products may also perturb surface integrity, though its long-term impact requires further study.Mechanical factors like dental prostheses, sharp teeth, or bruxism induce localized hyperkeratosis—a compensatory thickening that protects vulnerable tissue but may cause discomfort or ulceration if prolonged. Conversely, dehydration reduces mucosal hydration, weakening the natural barrier effect of keratinization and increasing susceptibility to trauma.
The keratinized oral mucosa is far more than a static tissue layer—it is a dynamic, stress-adapted interface that preserves oral function and health through its robust, keratinized structure.From shielding against mechanical and microbial challenges to guiding disease diagnosis and treatment, its role is indispensable. Continued research into its biology and clinical implications promises deeper insight into oral mucosal resilience, reinforcing its status as a cornerstone of oral physiology and preventative care.



Related Post

Chico Now: Elevating Local Living Through Smart Community Innovation

Douglas Oliver Cowley’s Final Farewell: A Community's Touchstone in Alamogordo’s Obituary Tradition
Meg Ryan Bio Wiki Age Height Husband Top Gun Movies and Net Worth

