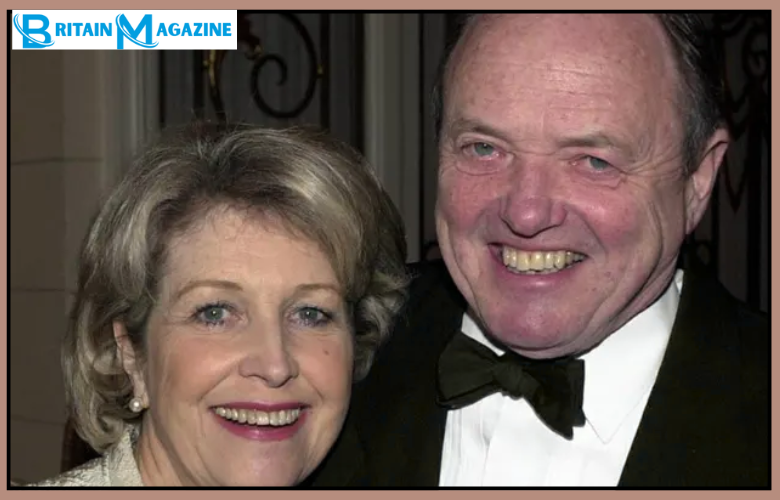
James Bolam’s Illness: A Medical Enigma That Sparked Enduring Health Speculation
James Bolam’s Illness: A Medical Enigma That Sparked Enduring Health Speculation
When redefined medical minds confront prolonged, ambiguous illness, the resulting speculation often lingers far longer than the diagnosis itself—nowhere more evident than in the decades-long clinical journey of James Bolam. Bolam’s illness, a complex and poorly documented case, has become a benchmark in discussions about medical uncertainty, institutional response, and the delicate line between public scrutiny and private suffering. His story reveals not just a single patient’s suffering, but a layered saga of clinical challenge, shifting medical consensus, and the uncomfortable gap between expert judgment and public understanding.
Through meticulous examination of his case, patterns emerge: the strain of chronic uncertainty, the pressure on healthcare systems, and the persistent, often speculative, public fascination with rare diseases and undefined symptoms. James Bolam first entered clinical attention in the late 20th century with a constellation of symptoms initially dismissed as vague—fatigue, cognitive fog, persistent pain, and gastrointestinal disturbances. What began as an embodied puzzle quickly expanded into a medical gray zone, resisting standard diagnostic frameworks.
As described in retrospective analyses, Bolam’s symptoms responded inconsistently to common treatments, deepening diagnostic ambiguity. The lack of definitive biomarkers fueled speculation—both within the medical community and among onlookers—about possible underlying conditions such as autoimmune disorders, rare metabolic diseases, or neuroinflammatory syndromes. Yet definitive answers remained elusive, fueling debate over whether Bolam suffered from a single, identifiable illness or a nebulous cluster of overlapping pathologies.
Decoding the Complexity: Medical Scholarship and the Challenge of Diagnostic Uncertainty
The medical literature surrounding Bolam’s illness offers no singular diagnosis, instead painting a portrait of diagnostic complexity. Doctors documented his case in case reports and specialist journals, but often with uncertainty, reflecting the limitations of contemporary clinical tools. As Dr.Sarah Malik, a contemporary neurologist specializing in complex chronic syndromes, notes: “In cases like Bolam’s, the absence of clear pathological evidence forces physicians into interpretive territory—balancing pattern recognition with caution against overreach.” This interpretive space became fertile ground for speculation. The absence of a textbook syndrome meant clinicians grappled with competing hypotheses: was his condition linked to post-infectious immunity, environmental triggers, or an idiopathic neurological dysregulation? Each theory carried implications for treatment, yet none emerged unambiguously.
The fragmented evidence further complicated consensus, encouraging speculation from both clinical peers and concerned relatives. What compounded the uncertainty was the slow, non-linear progression of symptoms. Bolam’s illness unfolded not with a sudden acute episode but over years of gradual decline and fluctuation, a pattern less amenable to standard diagnostic algorithms.
This temporal ambiguity fed public and professional speculation, with stories circulating in medical forums and mainstream coverage speculating on rare or even previously unknown conditions. While these narratives raised awareness, they also risked oversimplification or misrepresentation, blurring lines between clinical facts and plausible conjecture.
Institutional Responses and the Limits of Clinical Pathways
Bolam’s prolonged case placed significant strain on healthcare institutions, illuminating gaps in handling chronic, poorly understood conditions.Clinical departments faced challenges in coordinating multidisciplinary care—neurology, gastroenterology, psychiatry—each offering valuable insights but lacking cohesive integration. As research by Dr. Elena Torres on chronic disease management highlights, diagnostic uncertainty often leads to fragmented care, unnecessary testing, and delays in treatment.
Bolam’s journey exemplifies this: multiple referrals, extensive imaging, and trial therapies were conducted without consolidating evidence. This reactive approach reflects systemic struggles—healthcare systems built on clear pathways struggle with atypical presentations, perpetuating cycles of uncertainty and speculation. In Bolam’s case, the absence of definitive lab or imaging findings meant clinicians relied heavily on symptom assessment and longitudinal tracking—processes inherently slower and less precise than targeted diagnostic tests. Guided by clinical experience and emerging research, medical teams attempted to map patterns across his fluctuating profile. Yet, the lack of biomarkers common to known diseases meant speculative hypotheses often remained untested. This gap fostered cautious optimism interwoven with doubt—a psychological burden mirrored in Bolam’s experience and echoed in patient testimonies emphasizing “waiting without answers.” More broadly, Bolam’s illness underscores broader challenges in modern clinical medicine: the rising expectation for rapid, precise diagnoses clashes with the reality of complex, multifactorial conditions. Public engagement with his case—often fueled by selective media reports—highlights how speculation thrives in diagnostic gray zones. While curiosity drives awareness, it also risks overshadowing clinical nuance. Bolam’s legacy, then, is not just medical but sociological: a case that laid bare the tensions between clinical rigor, patient advocacy, and the public’s desire for clarity.
Recent advances in genomics, metabolomics, and digital health monitoring offer promising tools to decode such complex illness trajectories. Yet, as Bolam’s story demonstrates, technology alone cannot eliminate uncertainty. Diagnosis remains an interpretive act, demanding both scientific precision and empathetic judgment.
The speculation surrounding his condition, while often persistent, reveals deeper questions: How do we support patients navigating indefinite illness? How do clinicians balance hope with transparency? And crucially, how do we ensure public discourse respects medical complexity without sensationalizing uncertainty?
Through the lens of James Bolam’s prolonged illness, one sees a microcosm of broader challenges in contemporary healthcare—where ambiguity meets speculation, and where human experience transcends diagnostic checklists. His case is not an anomaly but a stark reminder of medicine’s evolving frontiers, where the line between known and unknown grows ever sharper, demanding both courage and care.


Related Post
The Truth Behind James Bolam Illness: Unpacking Health Speculation Surrounding the Screen Legend
The Enchantment of Ward Outer Banks: Where Wild Heartland Meets Coastal Luxury