HER2-Negative Breast Cancer: Unlock Your Diagnosis and Take Informed Control
HER2-Negative Breast Cancer: Unlock Your Diagnosis and Take Informed Control
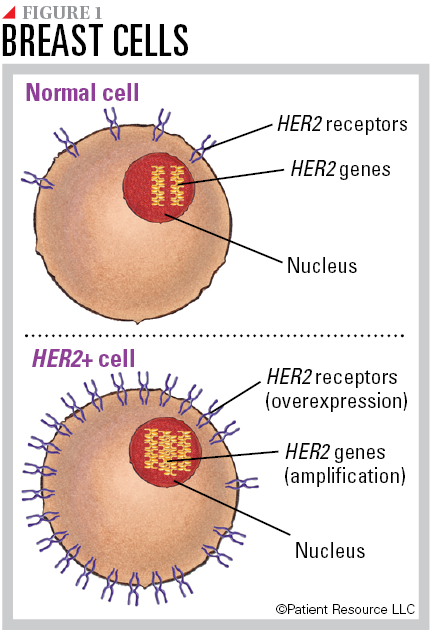
People newly diagnosed with HER2-negative breast cancer face critical decisions shaped by biology, treatment options, and long-term outlook—info that demands both precision and compassion. Unlike HER2-positive cancers, which respond to targeted therapies, HER2-negative tumors arise in the absence of this specific receptor, making access to effective treatment dependent on nuanced clinical evaluation and tailored strategies. With up to 80% of all breast cancers classified as HER2-negative, understanding the full spectrum of disease subtypes, molecular characteristics, and personalized management is essential for both patients and caregivers.
Although HER2-negative breast cancers lack overexpression or amplification of the HER2 receptor, subtle genomic variations influence response to therapy and disease progression. For many patients, distinguishing between Luminal and Basal-like subtypes informs prognosis and treatment, highlighting the need for comprehensive genomic testing. “The term ‘HER2-negative’ masks a wave of molecular diversity,” notes Dr.
Elena Rodriguez, a molecular oncologist at Memorial Sloan Kettering. “Accurate subtyping is the foundation for precision oncology.” From Hormone Receptor Status to Targeted Therapy: The Treatment Maze Treatment pathways for HER2-negative breast cancer hinge dramatically on additional receptor status, namely estrogen and progesterone hormone receptors (ER/PR). Tumors are classified as Luminal A (ER+/PR+, HER2−, low-grade) or Luminal B (ER+/PR+, HER2− or +, higher proliferation), each dictating different therapeutic approaches.
Luminal A cancers typically respond best to hormone therapy alone, such as tamoxifen or aromatase inhibitors, with 5-year survival rates often exceeding 90% when treated early. In contrast, Luminal B cancers—regardless of HER2 status—require aggressive combination strategies, frequently integrating chemotherapy with targeted hormonal agents. For HER2-negative cancers without strong hormone receptor expression, the options widen but demand careful stratification.
Historically, the absence of HER2 made these cancers harder to treat, but advances in chemotherapy regimens and emerging therapies have transformed outcomes. Today, adjuvant chemotherapy remains a cornerstone, often followed by endocrine therapy to minimize recurrence. Parallel progress in immunotherapy and CDK4/6 inhibitors has further refined treatment, especially for advanced or high-risk cases.
“Even when HER2 is negative, tumors often express other targets or vulnerabilities,” explains Dr. Marcus Lin, a breast cancer specialist at Kaiser Permanente. “Identifying these allows clinicians to build smarter, more effective regimens.” Beyond Standard Biomarkers: The Role of Genomic Testing and Emerging Biomarkers While hormone and HER2 status guide initial treatment, genomic profiling is increasingly vital in navigating HER2-negative breast cancer’s complexity.
Tests like Oncotype DX or MammaPrint assess gene expression patterns to estimate recurrence risk and chemotherapy benefit—particularly useful in Luminal A and B subtypes where endocrine therapy may suffice. For aggressive or node-positive disease, next-generation sequencing uncovers rare mutations that may open doors to clinical trials or targeted drugs. Emerging biomarkers such as PIK3CA mutations, cronic alterations, and tumor mutational burden are shape-shifting care.
A patient with Luminal B cancer harboring a PIK3CA mutation might respond better to combined endocrine and PI3K inhibitor therapy, while those with high mutational load could benefit from immune checkpoint inhibitors in clinical trial settings. “Genomics turns breast cancer from a one-size-fits-all disease into a personalized journey,” says Dr. Lin.
“For HER2-negative patients, this means a targeted strategy rooted in evidence, not guesswork.”
Staging remains integral to prognosis and treatment planning. The Massey Staging System classifies HER2-negative breast cancers from Stage I to IV, with each stage influencing the intensity of therapy and expected outcomes. Early-stage disease (I–II) often responds well to surgery and adjuvant hormonal or chemo regimens, while metastatic disease (Stage IV) requires systemic approaches, including novel agents and palliative strategies focused on quality of life.
Shared decision-making between patient and care team is paramount. Managing anxiety around diagnosis means translating clinical data into clear, actionable insights—not just statistics, but realistic expectations and supportive options. Targeted therapies have reduced reliance on blunt chemotherapy, offering better symptom control and fewer side effects in many cases.
Yet progression remains possible, underscoring the need for vigilant monitoring and adaptive treatment plans.
Navigating a HER2-negative breast cancer diagnosis is a journey defined by evolving science, individual biology, and empowered choice. As molecular understanding deepens, so too does the ability to tailor care that maximizes survival and preserves wellness—transforming diagnosis from a moment of fear into one of informed hope.];
Understanding HER2-negative breast cancer is no longer just a medical inquiry; it’s a call to precision, empathy, and lifelong partnership in healing.

:max_bytes(150000):strip_icc()/VWH-MiraNorian-Her2andBreastCancer-Standard-449f3c7a4c39449bad46f30c89bd16c6.jpg)

Related Post
Eric Bischoff Demolishes Tony Khan While Explaining Why He Lost All Respect For Him
Heres The Real Reason Nhlanhla Nciza Divorced Her Husband After 15 Years and Four Children
Exclusive Analysis: Selena Gomez On Playboy Magazine Cover Discussion
Kemani Alexander Age Wiki Net worth Bio Height Girlfriend

