GLP-1 Inhibitors: Everything You Need To Know
GLP-1 Inhibitors: Everything You Need to Know — From Weight Loss Breakthroughs to Diabetes Breakthroughs, these powerful medications are reshaping modern medicine by targeting one of the body’s most influential hunger-regulating systems. Originally developed to treat type 2 diabetes, GLP-1 receptor agonists now dominate headlines as frontline tools in obesity management, offering sustained weight reduction and improved metabolic health. With growing scientific validation and expanding clinical use, understanding how these drugs work, their benefits, risks, and real-world impact is essential for patients, clinicians, and anyone following innovations in metabolic medicine.
What Are GLP-1 Inhibitors and How Do They Work?
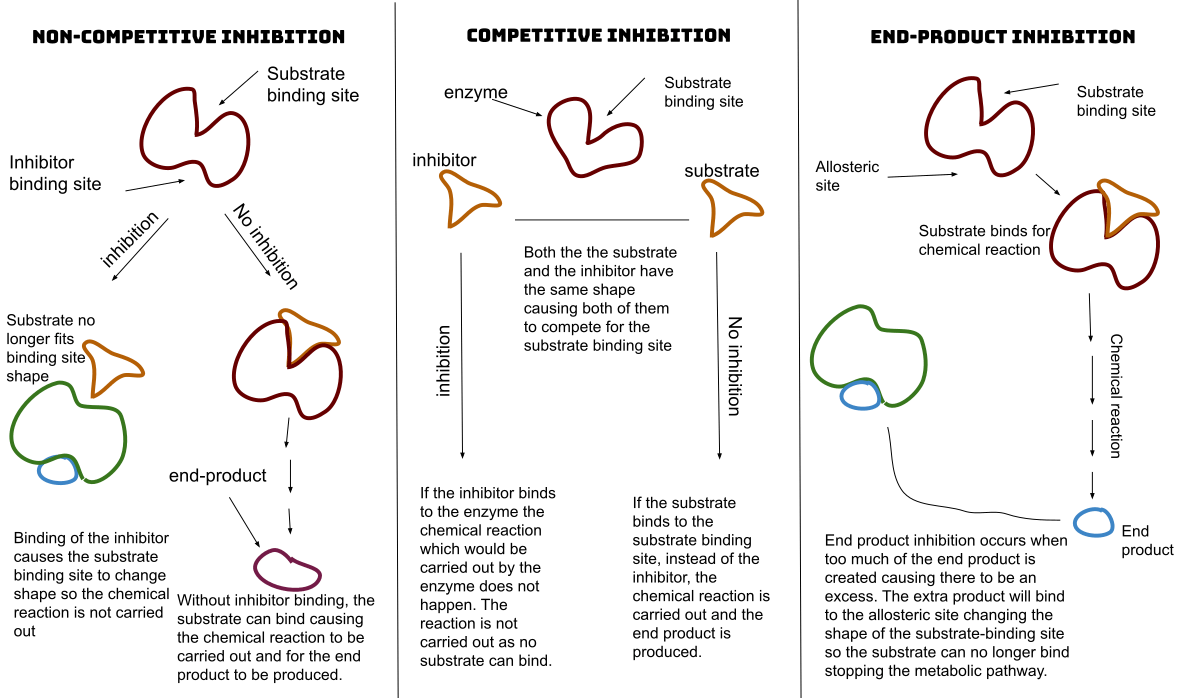
GLP-1 stands for glucagon-like peptide-1, a naturally occurring hormone produced in the gut in response to food intake.This hormone plays a key role in regulating blood sugar, appetite, and gastric emptying by signaling the brain to reduce hunger and increase satiety. GLP-1 inhibitors mimic this action by blocking the degradation of GLP-1, extending its effects and amplifying its metabolic benefits. The active ingredients in these medications include semaglutide (marketed as Ozempic and Wegovy), liraglutide (Saxenda), and tirzepatide (Mounjaro), each targeting GLP-1 receptors with precision.
By prolonging satiety and slowing digestion, these drugs create a natural reduction in calorie intake without suppressing the appetite through stimulant pathways. “GLP-1 inhibitors work with the body’s own physiology, making them preferable to older weight-loss drugs with more adverse side effects,” explains Dr. Elena Torres, an endocrinologist at the Center for Metabolic Medicine.
“They don’t just reduce hunger—they enhance the body’s natural regulation of food intake.”
In diabetes treatment, GLP-1 agonists lower blood glucose by stimulating insulin release when sugar is high and dampening glucagon—an opposing hormone that raises blood sugar. This dual action improves glycemic control with minimal risk of hypoglycemia. For obesity, the focus shifts to appetite suppression and sustained energy balance.
Clinical trials show participants using these medicines lose 10% to 15% of body weight over a year, with some achieving losses exceeding 20%. The mechanism isn’t merely caloric restriction—it’s neurobiological modulation. Brain imaging reveals GLP-1 inhibition dampens activity in regions associated with food reward and craving, effectively rewireing the brain’s response to food cues.
Clinical Evidence: Trials That Redefined Obesity and Diabetes Care
The landmark trials behind GLP-1 inhibitors are nothing short of transformative.The SCALE trial (Semaglutide Treatment and Control in Obesity) demonstrated that weekly semaglutide led to an average weight loss of 15.2% from baseline in participants with obesity or overweight and at least one weight-related comorbidity. Another pivotal study, the STEP (Semaglutide Treatment Effect in People with Obesity) trial series, confirmed consistent weight reduction between 12% and 18% over 68 weeks, with cardiovascular benefits observed in high-risk populations. For diabetes patients, the LEADER trial revealed that liraglutide reduced major cardiovascular events—including heart attacks and strokes—by 13% in those with existing cardiovascular disease.
Beyond semaglutide and liraglutide, tirzepatide has induced clinically significant weight loss up to 20.6% in early-stage trials, blurring the line between diabetes and obesity therapies. These results have prompted the FDA and EMA to expand approvals, making GLP-1 inhibitors a cornerstone in updated clinical guidelines for both conditions. “The data don’t lie—GLP-1 inhibitors are rewriting expectations,” says Dr.
Torres. “They’re not a quick fix, but a sustainable, physiological shift in how the body manages food and energy.”
Usage, Safety, and Real-World Considerations
GLP-1 inhibitors are predominantly administered via subcutaneous injection, with once-weekly formulations like Ozempic and Wegovy offering convenient dosing. Oral liraglutide (Saxenda) requires twice-daily administration.Common side effects include nausea, vomiting, diarrhea, and constipation—symptoms typically mild and transient, often resolving as the body adapts. “The most frequent complaint we see is gastrointestinal discomfort, usually at initiation,” notes Dr. Raj Patel, a primary care physician managing metabolic patients.
“Starting low and titrating slowly minimizes these effects while maximizing adherence.” Serious risks are rare but exist. Pancreatitis and gallbladder disease have been reported, while concerns about thyroid C-cell tumors—observed in rodent studies—remain under investigation in humans; no conclusive evidence of harm has emerged in humans thus far. Blood pressure fluctuations and kidney function monitoring are recommended, especially in patients with pre-existing conditions.
Long-term safety data continues to accumulate, with 52-week trials indicating sustained weight loss and metabolic benefits without loss of efficacy over time. Patient experiences vary: one user described semaglutide as “a game-changer that ended cycling of weight gain and loss,” while another noted initial nausea but eventual normalization. These variations underscore the need for personalized treatment—effective for many, but not universally optimal.
Regular follow-ups, lifestyle integration, and realistic expectations remain essential. “GLP-1 inhibitors work best when paired with diet, exercise, and behavioral support,” stresses Dr. Torres.
“They’re powerful tools, but not replacements for holistic metabolic health.”
As research expands, newer dual agonists like tirzepatide—targeting both GLP-1 and GIP receptors—are setting new benchmarks, with potential to further enhance efficacy and address unmet needs. The GLP-1 inhibitor revolution isn’t a passing trend; it represents a paradigm shift in how we approach chronic metabolic conditions. By harnessing the body’s own regulatory systems, these drugs deliver not just weight loss, but improved heart health, blood sugar control, and quality of life.
For clinicians and patients alike, understanding the science, applications, and practical nuances of GLP-1 inhibitors is key to unlocking their full potential.”
Looking Ahead: The Future of GLP-1 Therapeutics
The future is already unfolding. Clinical pipelines include next-generation GLP-1 analogs with even longer half-lives, potentially reducing dosing frequency. Combination therapies pairing GLP-1 agonists with other metabolic agents—such as amylinomimetics—are in development, aiming for synergistic effects on appetite and glucose control.Meanwhile, digital health integration—tracking adherence, symptoms, and outcomes via apps—promises to optimize treatment personalization. As insurance coverage improves and guidelines evolve, GLP-1 inhibitors are poised to become standard care for obesity and high-risk diabetes, reshaping preventive medicine. With ongoing research validating long-term safety and expanding indications, GLP-1 inhibitors are more than a treatment—they are a transformative force in metabolic health, offering lasting benefits rooted in physiology rather than suppression.


Related Post