For Medical Term: The Pathophysiology of Chronic Obstructive Pulmonary Disease
For Medical Term: The Pathophysiology of Chronic Obstructive Pulmonary Disease
Chronic Obstructive Pulmonary Disease (COPD) remains one of the most prevalent and underdiagnosed respiratory conditions globally, affecting over 251 million people according to the Global Burden of Disease Study. Defined by persistent airflow limitation due to chronic lung inflammation, COPD encompasses diseases such as emphysema and chronic bronchitis, driven primarily by long-term exposure to irritants like cigarette smoke. Understanding its pathophysiology reveals a complex interplay between environmental triggers, immune response dysregulation, and structural changes in the lungs—processes that collectively impair breathing and diminish quality of life.
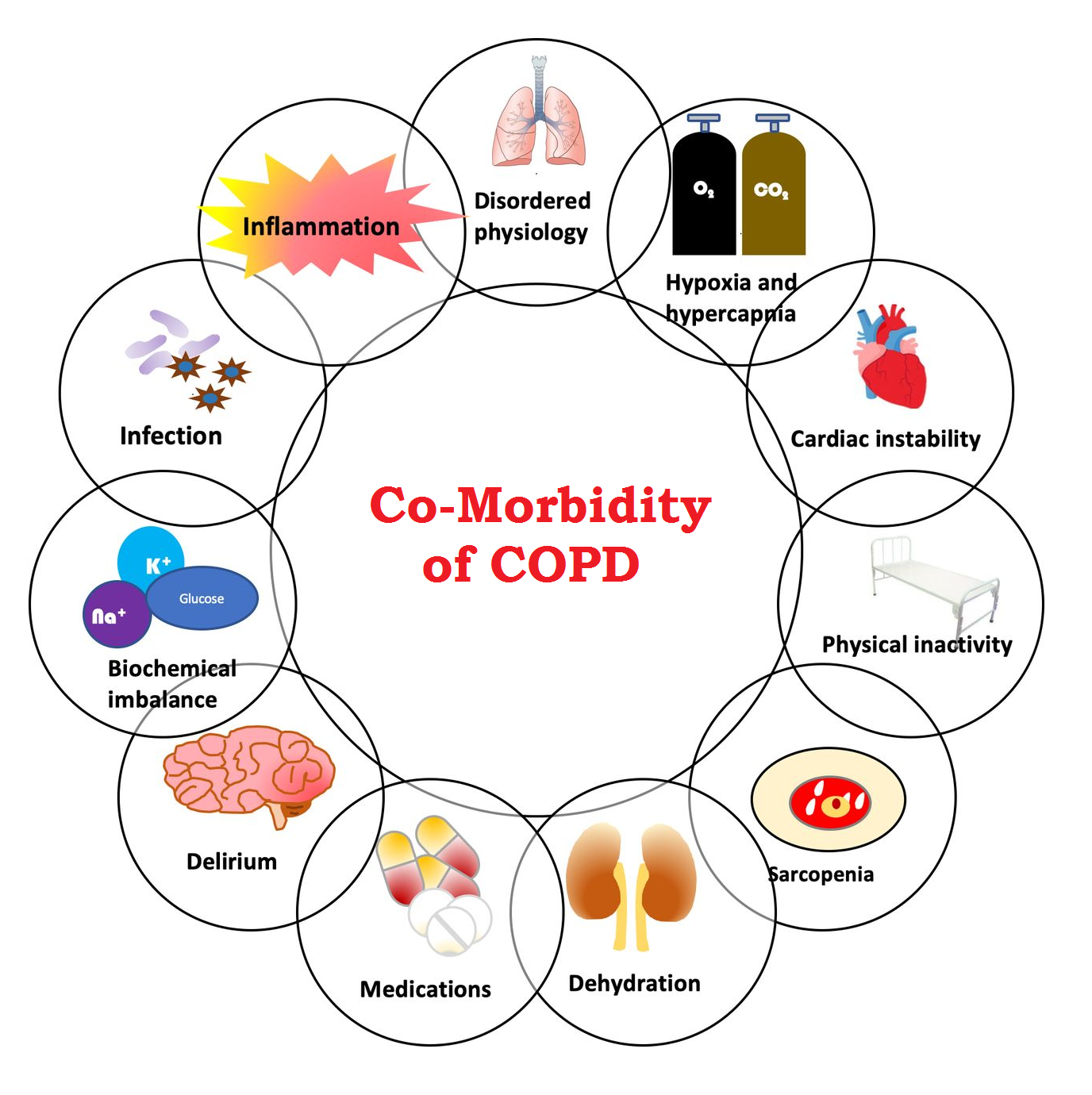
At the core of COPD lies chronic inflammation, initiated by inhaled harmful particles that activate immune cells such as macrophages and neutrophils in the airways and alveoli. These cells release a cascade of pro-inflammatory cytokines—including tumor necrosis factor-alpha (TNF-α), interleukin-8 (IL-8), and interleukin-6 (IL-6)—perpetuating tissue damage. This inflammatory environment disrupts normal repair mechanisms and promotes oxidative stress, a key driver in lung degradation.
“Inflammation in COPD evolves from a protective response to a destructive force,” explains Dr. Elena Rodriguez, Senior Pulmonologist at Johns Hopkins Medicine. “Once established, it resists resolution and accelerates structural remodeling.”
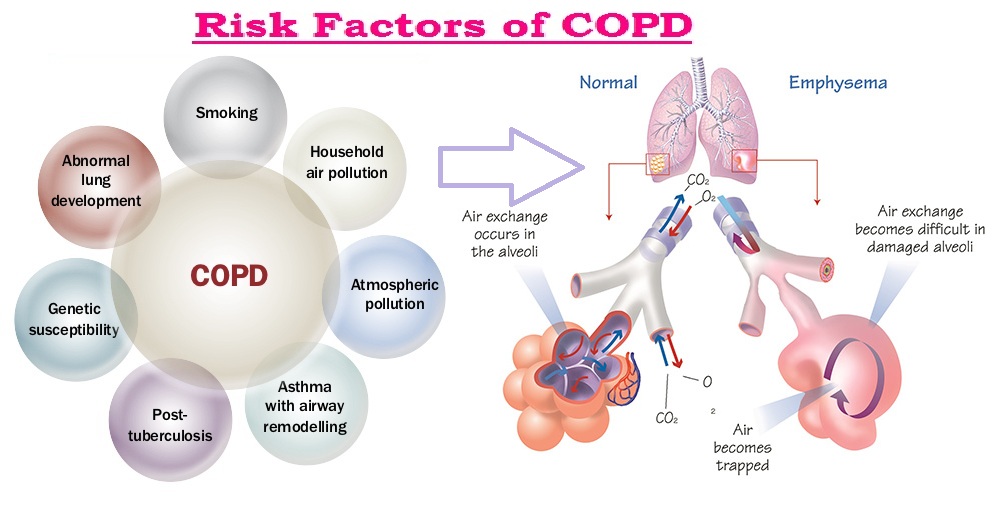
Structural changes follow inflammation, including thickening of airway walls, mucus hypersecretion, and destruction of alveolar walls—most notably in emphysema.
Alveolar sacs lose elasticity and surface area, reducing gas exchange efficiency. “The loss of alveolar attachments creates weak, overinflated lungs that collapse easily during exhalation,” notes Dr. Marcus Chen, a respiratory pathologist.
This obstruction results in air trapping, hyperinflation, and increased work of breathing, hallmark features of advanced COPD. Additional structural features include fibrosis in smaller airways, contributing to fixed airflow obstruction that doesn’t resolve with bronchodilators.
The clinical manifestations stem directly from these underlying pathophysiological processes.
Patients typically report progressive dyspnea (shortness of breath), chronic cough, and excessive sputum production—symptoms that worsen over years. As mucus plugs obstruct narrowed airways and lung elasticity declines, oxygenation drops and carbon dioxide retention becomes common, potentially leading to respiratory acidosis. Severe cases can trigger acute exacerbations, often triggered by infections or increased pollution, which dramatically worsen lung function within days.
“Exacerbations are not just flare-ups—they accelerate disease progression,” warns Dr. Chen. “Each episode represents a critical juncture where intervention can either slow or hasten decline.”
Risk factors extend beyond smoking, though it accounts for 85–90% of COPD cases.
Long-term exposure to occupational dusts, secondhand smoke, indoor biomass fuels, and air pollution significantly increase susceptibility. Genetic factors also play roles; for example, alpha-1 antitrypsin deficiency—a rare inherited condition—impairs protease inhibitor balance, accelerating lung destruction independently of smoking. Identifying at-risk individuals early through spirometry testing enables timely intervention, such as smoking cessation and environmental controls, which remain cornerstones of management.
Diagnosis relies on clinical evaluation, spirometry, and imaging. A post-bronchodilator FEV1/FVC ratio below 0.70 confirms persistent airflow limitation, with emphysema typically identified via high-resolution CT (HRCT) showing low-attenuation gradients and visible wall thickening. Biomarkers including C-reactive protein (CRP) and fractional exhaled nitric oxide (FeNO) provide insight into inflammation severity but do not replace functional testing.
“Spirometry remains the gold standard,” emphasizes Dr. Rodriguez, “because it quantifies disease severity and guides personalized therapy.”
Treatment strategies focus on symptom relief, slowing progression, and preventing exacerbations. Pharmacological approaches include bronchodilators (long-acting beta-agonists and muscarinic antagonists) to relax airway smooth muscle and inhaled corticosteroids to reduce inflammation—though response variability underscores the need for tailored regimens.
Pulmonary rehabilitation, rich in exercise, breathing techniques, and education, improves functional capacity and mental well-being. Oxygen therapy corrects hypoxemia in advanced disease, while surgical options—such as lung volume reduction or transplant—remain reserved for severe, refractory cases. Vaccinations against influenza and pneumococcus mitigate infection risks, a leading cause of hospitalization and mortality.
Emerging research highlights novel targets, including anti-cytokine therapies and anti-remodeling agents aimed at interrupting the inflammatory cascade and alveolar destruction. Anti-TNF and IL-17 inhibitors are under investigation for selected patients, though clinical translation remains limited. Advances in regenerative medicine explore stem cell therapy and tissue engineering to repair damaged lung architecture—offering hope for future breakthroughs.
“COPD is no longer considered an inevitable consequence of aging or smoking,” states Dr. Chen. “With deeper mechanistic understanding, we are moving toward interventions that directly modify underlying pathophysiology, not just manage symptoms.”
Worldwide, COPD underscores urgent public health challenges.
High prevalence rates strain healthcare systems, particularly in low- and middle-income countries with rising smoking rates and increasing air pollution. Yet, its complexity—spanning environmental, molecular, and clinical domains—is driving a paradigm shift from reactive care to proactive, precision-based management. By integrating pathophysiological insights with patient-centered strategies, the medical community aims to transform COPD from a debilitating chronic condition into a condition with prolonged, dignified living.
Understanding COPD through its pathophysiology not only enhances diagnostic accuracy and therapeutic precision but also fuels innovation toward curative possibilities. As research accelerates and global awareness grows, the future holds promise for reshaping the trajectory of this widespread disease—one molecule, one cell, and one breath at a time.


Related Post

How Tall Is Elon Musk? Decoding the Surface of a Titan
Unlocking Innovation: How Aanews1 Revolutionizes Global News Consumption with Real-Time, Multi-Platform Reporting
Scrutinizing the Origins of Huda Love Island Ethnicity
Ultimate Guide to the Best Alternatives for Omegle Chat Platforms – Safe, Dynamic, and Anonymity-Ready Chat Spaces for Every User

