Engineering Precision: How PDT is Revolutionizing Treatment and Redefining Medical Standards
Engineering Precision: How PDT is Revolutionizing Treatment and Redefining Medical Standards
Salvation lies in the control — in the meticulous orchestration of timing, biology, and delivery. Among the most innovative frontiers in modern medicine is Photodynamic Therapy (PDT), a technique leveraging light, photosensitizing agents, and oxygen to selectively destroy diseased cells with unprecedented precision. Now, emerging breakthroughs in Patient-Derived Tissue (PDT) models are not only refining treatment protocols but fundamentally transforming how clinicians predict outcomes, personalize therapies, and accelerate translational research.
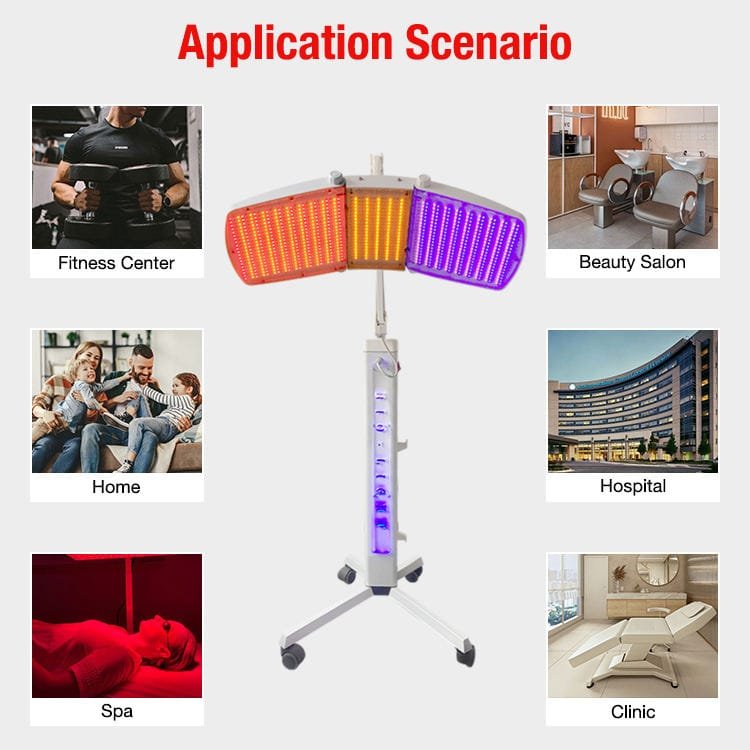
From cancer care to chronic skin disorders, this synergy between biology and technology is sharpening the edge of medicine. PDT operates on a deceptively simple principle: a photosensitizer drug accumulates in target cells, then when exposed to a specific wavelength of light, it generates reactive oxygen species that trigger cell death. But its real power emerges in customization — especially when derived directly from a patient’s own tissues.
Patient-Derived Tissues (PDT samples), grown in controlled environments that mimic native physiology, offer an unparalleled window into individual responses. “This shift from generic models to personalized tissue platforms marks a quantum leap,” says Dr. Elena Marquez, a bioengineer at the Institute for Translational Photomedicine.
“We’re no longer testing drugs on generic cell lines — we’re using a patient’s living tissue to map how their unique biology reacts.” ### The Science Behind Patient-Derived PDT Tissues Creating PDT-compatible tissues begins with meticulous isolation and cultivation. Tissue biopsies — from tumor margins, skin lesions, or pre-cancerous samples — are processed to preserve cellular architecture and functionality. Advanced bioprinting and organoid technology allow scientists to reconstruct these tissues layer by layer, replicating microenvironmental cues such as blood flow, oxygen gradients, and extracellular matrix composition.
> “The key is fidelity,” explains Dr. Raj Patel, lead researcher in a 2023 study on PDT response modeling. “We’re not just growing cells — we’re growing a functional microcosm where we can shuttle a light probe, trigger photodynamic reactions, and measure real-time cytotoxicity.” This level of control enables precise calibration of light dosage, drug concentration, and exposure duration — variables critical to PDT’s success.
Step-by-step development includes: - **Tissue procurement and preservation** under sterile, low-oxygen conditions to maintain viability. - **3D bioprinting or organoid formation** using patient-specific extracellular matrix proteins and growth factors. - **In vitro photosensitizer delivery** tailored to mimic pharmacokinetics observed in human plasma.
- **Real-time monitoring** via fluorescence imaging and oxygen sensors to track reactive oxygen species (ROS) generation. - **Post-treatment analysis** of viability, repair mechanisms, and residual activity using high-content microscopy. These tissues now serve dual roles: as diagnostic tools and therapeutic testing platforms, ensuring that PDT protocols are optimized before clinical application.
### Transforming Cancer Care Through Personalized PDT In oncology, PDT’s precision is especially transformative. Unlike conventional radiation or chemotherapy, PDT spares surrounding healthy tissue, reducing side effects and enabling repeated treatments. Yet response varies widely among individuals due to genetic heterogeneity, tumor microenvironment, and metabolic differences.
Patient-Derived PDT Tissues bridge this gap. For example, in head and neck cancers, clinicians now use tumor organoids derived from a patient’s biopsy to simulate PDT efficacy. “We test dozens of photosensitizer doses and light energies on these miniature tumors,” says Dr.
Marquez. “Within days, we identify the regimen most likely to clear the tumor without damaging adjacent nerves or muscle.” > “One patient’s tumor may shrink with 10 millijoules per square centimeter of light, while another requires double that dose — all without prior tissue damage,” she notes. “This level of personalization was impossible a decade ago.” Clinical trials increasingly validating PDT’s potential: a 2024 multicenter study found patient-matched PDT protocols improved local control rates by 18% compared to standard regimens in non-melanoma skin cancers.
Moreover, emerging evidence suggests PDT may stimulate anti-tumor immune responses, turning localized therapy into systemic advantage. ### Beyond Oncology: PDT in Chronic Diseases and Dermatology While cancer dominates current research, PDT’s utility extends into dermatology, ophthalmology, and inflammatory conditions. In psoriasis, for instance, PDT targeting hyperproliferative skin layers reduces scaling with minimal scarring.
In age-related macular degeneration, light-activated therapies are being refined to selectively eliminate dysfunctional retinal cells without harming healthy tissue. Patient-Derived Models enhance these applications by replicating disease-specific microenvironments. A 2023 trial in chronic ulcerative wounds used bioprinted dermal organoids derived from diabetic patients to tailor PDT dosing, resulting in accelerated healing and reduced infection risk—outcomes unattainable with generic models.
“Each PDT model tells a unique biological story,” says Dr. Marquez. “Harnessing that story means delivering therapies that fit the patient, not the average—making treatment smarter, safer, and more effective.” ### Challenges and the Road Ahead Despite rapid progress, hurdles remain._TUMOR heterogeneity_, variable photosensitizer uptake, and light penetration in deep tissues limit PDT’s reach.
Standardizing tissue sourcing, optimizing delivery hardware, and integrating real-time imaging feedback are active areas of research. Regulatory frameworks, too, must evolve to accommodate personalized PDT products, balancing innovation with patient safety. Yet momentum is building.
AI-driven modeling is accelerating tissue response predictions; novel photosensitizers with deeper tissue penetration and longer active lifespans are under development; and portable light devices are enabling in-clinic, real-time PDT activation. Headline: Photodynamic Therapy (PDT) has evolved from a niche technique into a cornerstone of targeted treatment, but its true potential is unlocked through Patient-Derived Tissues (PDT) — living, biocompatible models that mirror individual biology. By personally mirroring disease architecture, these tissues enable clinicians to fine-tune light delivery, drug cocktails, and exposure timelines for maximum efficacy and mínima risk.
The evidence is compelling: in oncology, personalized PDT protocols boost tumor clearance while sparing healthy tissue. In dermatology, tailored therapies reduce side effects and accelerate healing. And across disciplines, PDT’s integration with patient-specific data heralds a new era where treatment is no longer guesswork but precision engineering.
As Dr. Patel concludes, “We’re not just treating disease — we’re adapting to the patient.” With continued investment and interdisciplinary collaboration, PDT powered by PDT models promises to redefine what’s possible in medicine, one patient at a time.



Related Post

What Time Is It in Pacific Daylight Time? Mastering the Clock Behind一 Pacific Daylight Time (PDT)
Pdt Time in Canada: Precise Zone Rules and What Time Zone Your Country Actually Observes
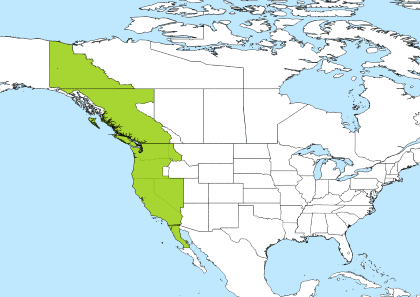
Pdt Time