DermIndex: The Medical Definition of Dermatology’s Precision in Clinical Practice
DermIndex: The Medical Definition of Dermatology’s Precision in Clinical Practice
When forensic precision meets dermatological diagnosis, the term DermOMedicalDefinition emerges not just as a clinical descriptor but as a vital tool in accurate patient care. Dermatology, a field defined by visual complexity and subtle morphological variation, relies heavily on universally standardized language to bridge gaps between clinician observation, diagnostic imaging, and inter-professional communication. DermOMedicalDefinition—though not a standalone clinical acronym—represents a synthesis of diagnostic clarity, taxonomic accuracy, and evidence-based terminology used to define skin conditions with precision, enabling reliable communication across specialties.
According to DermOMedicalDefinition, this concept encompasses structured descriptions that integrate clinical signs, histopathology, patient history, and etiological factors into a single, actionable diagnostic framework. The essence of DermOMedicalDefinition lies in its ability to transform subjective visual cues into objective, reproducible data. In dermatology, a diagnosis often hinges on nuanced features invisible to the untrained eye: subtle pigmentation changes, microscopic dermal patterns, or inflammatory architecture.
Without standardized definitions, discrepancies in interpretation can lead to misdiagnosis, delayed treatment, or inappropriate therapy. For example, the distinction between lichen planus and post-inflammatory hyperpigmentation may appear minor on the surface but carries profound implications for management—one responding to topical steroids, the other often requiring pigment cámara protocols or laser intervention.
Core Components of DermOMedicalDefinition: DermOMedicalDefinition integrates three foundational pillars:
- Clinical Description: Detailed imagery and symptomatology—such as erythema distribution, lesion morphology, and temporality—form the observational backbone.
This includes standardized descriptors like “violaceous, polygonal papules with collarette scaling” as defined in key DermOMedicalDefinition resources.
- Histopathological Correlates: Structural skin changes—from epidermal dysplasia to dermal infiltration—are mapped to microscopic findings. The definition process often references biopsy patterns and immunohistochemical markers critical to accurate classification.
- Contextual Etiology and Epidemiology: Beyond signs and tissues, DermOMedicalDefinition incorporates patient-specific risk factors—such as genetic predisposition or environmental triggers—and population-level incidence data, enriching contextual understanding.
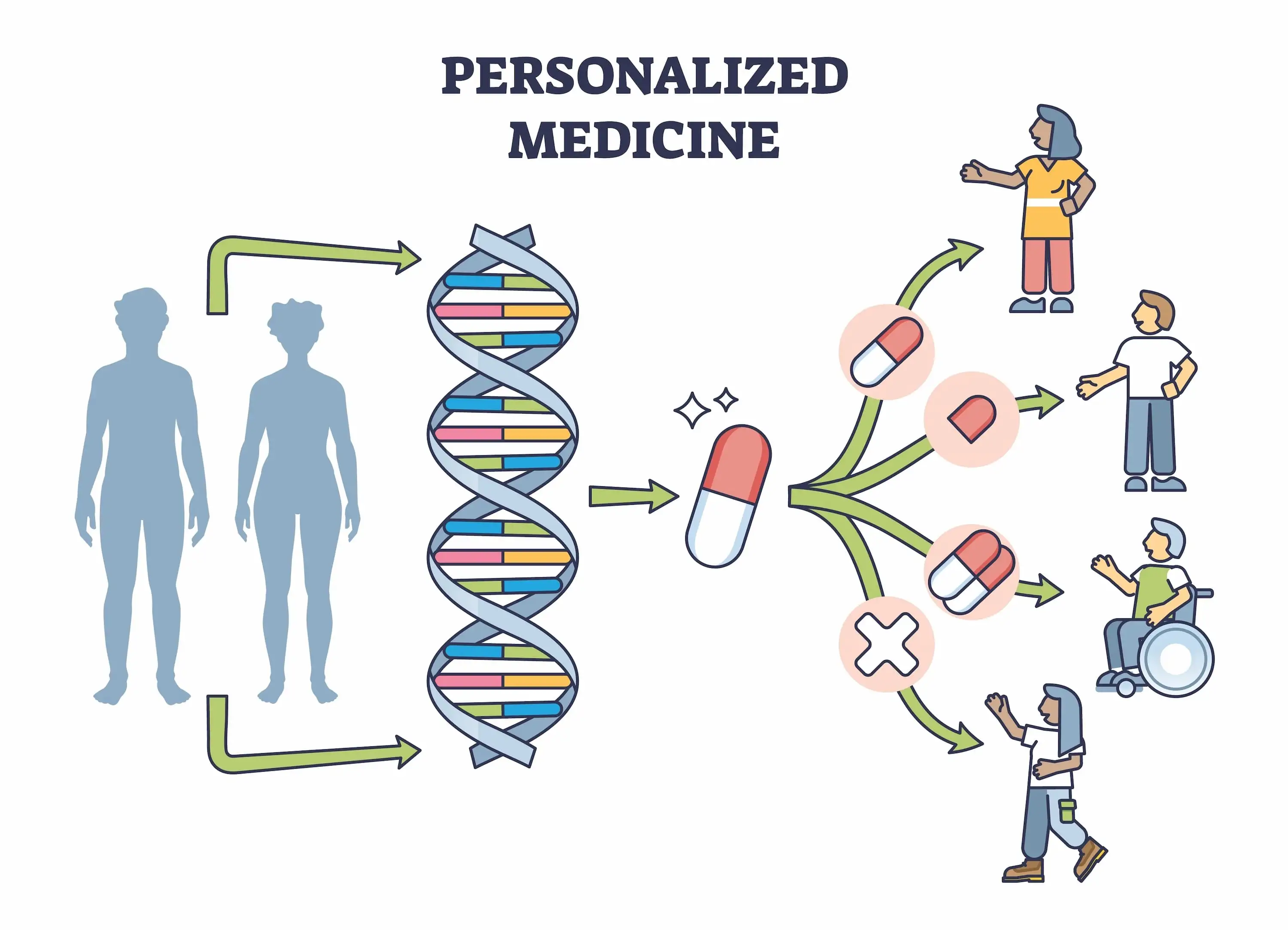
Key Diagnostic Features in Dermatological Contexts: Examining common conditions reveals how DermOMedicalDefinition sharpens diagnostic acuity. Take atopic dermatitis (AD), a chronic inflammatory disorder marked by pruritic, lichenified plaques. A DermOMedicalDefinition entry specifies not only the typical flexural distribution and skin RELM-α disruption but also contextual triggers—such as atopy history and filaggrin mutations—to guide personalized management.
Similarly, psoriasis relies on defining Waffen-type features: active plaques with silvery scales, nail pitting, and palmoplantar involvement—criteria essential for distinguishing plaque, guttate, and pustular subtypes. Another illustrative example is cutaneous lupus erythematosus, where a comprehensive definition accounts for interface dermatitis, basement membrane disruption, and specific autoantibody profiles to differentiate entrepithelial from fixed drug lupus. Each definition moves beyond isolated signs to synthesize pattern recognition with mechanistic insight.
This aligns with DermOMedicalDefinition’s core purpose: reducing ambiguity in a specialty where a single misinterpreted feature can derail treatment pathways.
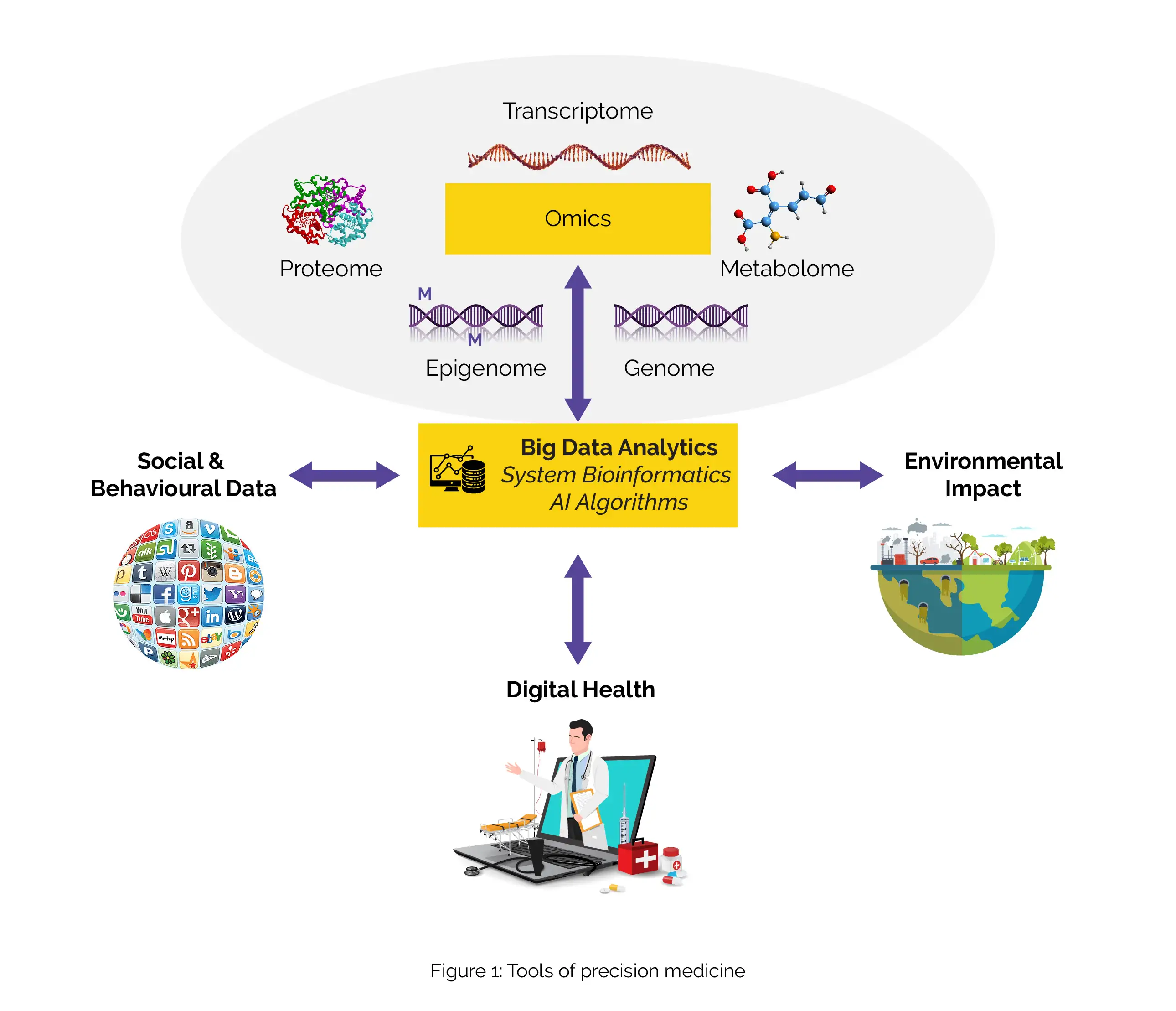
Evolution of Diagnostic Standardization: Historically, dermatological diagnosis depended on physician experience and descriptive shorthand, often leading to variability in interpretation. The emergence of standardized definitions—championed by organizations like the American Academy of Dermatology and supported by platforms formalizing DermOMedicDefinition—marks a critical evolution toward precision medicine.
These definitions serve dual roles: enhancing patient safety by minimizing diagnostic errors, and empowering multidisciplinary teams through shared reference points. In complex cases involving comorbidities or overlapping syndromes—such as lupus vulgaris mimicking squamous cell carcinoma—standardized terminology enables cross-specialty translation, facilitating timely biopsy, referral, and targeted therapy. Moreover, DermOMedicalDefinition supports digital integration: imaging algorithms, electronic health records, and AI-assisted diagnostics increasingly rely on structured data inputs.
By embedding diagnostic clarity at the definition level, dermatologists contribute to interoperable, patient-centered care ecosystems where data flows seamlessly across encounter points.
Broader Implications for Dermatology and Beyond: Beyond clinical practice, DermOMedicalDefinition strengthens research integrity and education. Standardized definitions enable precise case reporting in dermatology registries, enhancing the reliability of clinical trials and outcome studies.
For trainees, these definitions provide clear, consistent benchmarks, accelerating competency development. In public health, authoritative diagnostic frameworks support accurate surveillance of skin diseases—critical for tracking prevalence shifts, outbreak patterns, or emerging conditions like drug-induced lupus variants. The term transcends the clinic: in pathology labs, legal medicine (e.g., forensic dermatology), and global telehealth platforms, having a universally accepted DermOMedicalDefinition ensures diagnostic continuity, regardless of geographic or experiential background.
Ultimately, DermOMedicalDefinition represents more than a technical lexicon—it embodies a commitment to clarity, accuracy, and equity in dermatological care. By codifying the visible into structured, evidence-based knowledge, it empowers clinicians to diagnose with confidence, patients to access timely, targeted treatment, and researchers to build reliable


Related Post

Universal Life Church Ministries: Your Direct Path to Immediate Ordination
South African Currency Symbol Converter Exchange Rate

Beyond Daily Cafe: Critical Alternatives to Diversifying Your Horoscope Journey

