Bupropion: Unraveling Its Role as a Unique Antidepressant and Beyond
Bupropion: Unraveling Its Role as a Unique Antidepressant and Beyond
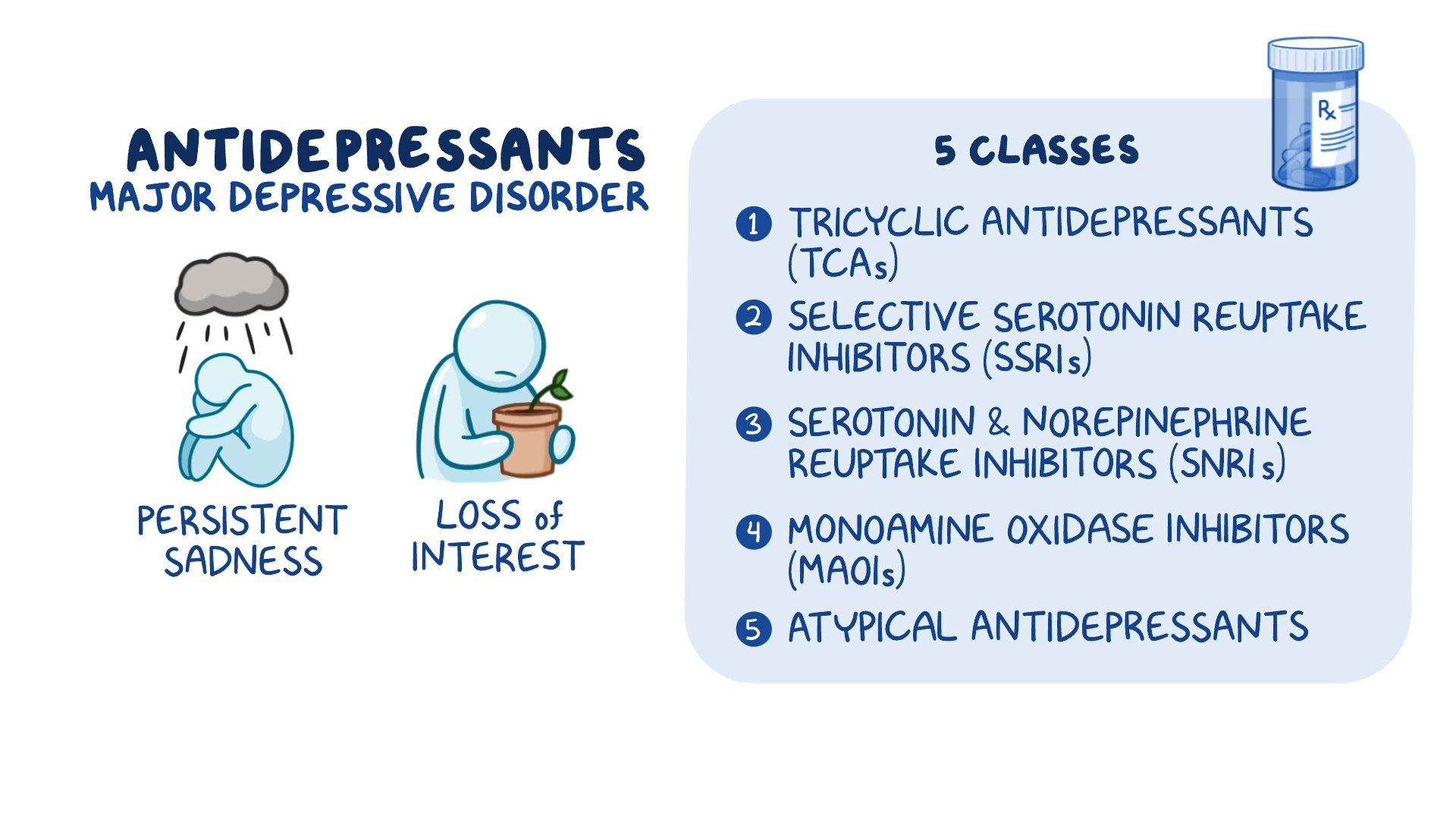
Bupropion stands out in the landscape of psychiatric medications as a non-benzodiazepine, norepinephrine-dopamine reuptake inhibitor (NDRI), offering a distinct mechanism that bridges antidepressant action with smoking cessation support. Unlike the selective serotonin reuptake inhibitors (SSRIs) that dominate the treatment of mood disorders, bupropion modulates two key neurotransmitters—norepinephrine and dopamine—contributing to its dual utility in managing depression and reducing nicotine addiction. “Bupropion doesn’t just lift the mood; it alters the brain’s reward circuitry,” notes Dr.
Elena Torres, a clinical neuropharmacologist. This unique profile makes it a versatile tool in both mental health and behavioral health settings.
Understanding Bupropion’s Place in Drug Classification
Bupropion belongs to a class of drugs known as norepinephrine-dopamine reuptake inhibitors (NDRIs), a category defined by its ability to block the reabsorption of norepinephrine and dopamine in the synaptic cleft.Unlike the tricyclic antidepressants (TCAs) that also inhibit norepinephrine but affect multiple receptors non-selectively, or SSRIs that target only serotonin, bupropion’s action is more targeted and receptor-specific. This selectivity underlies its favorable side effect profile and reduced anticholinergic burden—common issues with older antidepressant classes. The pharmacological distinction is clear: - **Mechanism**: Blocks dopamine and norepinephrine transporters without significant serotonin activity - **Types**: Achieved in two formulations—oral bupropion (used for mood and smoking cessation) and intravenous (used in acute withdrawal settings) - **Metabolism**: Primarily liver-metabolized via cytochrome P450 enzymes, particularly CYP2B6, influencing dosing and drug interactions “This targeted approach allows bupropion to address depression without triggering the common sexual side effects and weight gain linked to serotonin-specific agents,” states Dr.
Rajiv Mehta, a psychiatrist specializing in mood disorders. By preserving noradrenergic and dopaminergic tone, bupropion supports cognitive function and motivation—factors crucial in recovery from depression and sustaining abstinence from smoking.
From Antidepressant to Quit-Smoking Aid: A Multifaceted Role
Originally approved in the U.S.in 1985 as an antidepressant under the brand name Wellbutrin, bupropion carved a niche beyond mood stabilization when its off-label use for smoking cessation emerged in the 1990s. Clinical trials confirmed its efficacy: a landmark study in the New England Journal of Medicine demonstrated that bupropion doubled quit rates compared to placebo, making it a first-line option for nicotine dependence. “The drug dampens the dysphoric withdrawal symptoms and reduces cigarette cravings,” explains Dr.
Lisa Chen, a smoking cessation researcher. “It essentially normalizes the brain’s reward response to nicotine without psychoactive effects.” The extended-release oral formulation (Wellbutrin XL) is now FDA-approved specifically for smoking cessation, offering a once-daily dose that balances sustained therapeutic levels with minimal side effects. Bupropion’s mechanism in this context revolves around restoring dopamine in the mesolimbic pathway—targeting the brain’s reward system heavily implicated in addiction.
Concurrently, its norepinephrine activity enhances alertness and mood, countering the lethargy and irritability commonly experienced during quit attempts.
Safety Profile and Practical Use in Clinical Practice
While highly effective, bupropion is not without considerations. Its approved uses include major depressive disorder and off-label but well-supported indications for smoking cessation.The FDA blue box warning for increased risk of seizures at doses exceeding 450 mg/day underscores the importance of adherence to dosage guidelines—especially in patients with epilepsy or a history of seizures. Common side effects are generally mild and transient, including dry mouth, insomnia, anxiety, and, less frequently, decreased appetite or weight loss. Behavioral effects such as vivid dreams or restlessness are reported by 10–20% of users but often diminish over time.
“Most patients find the tolerability manageable, particularly when compared to stimulant-based cessation therapies,” notes Dr. Chen. Interactions with monoamine oxidase inhibitors (MAOIs) require strict avoidance due to the risk of serotonin- and dopamine-related adverse events, highlighting the need for careful medication reconciliation.
The dosing regimen reflects bupropion’s pharmacokinetic profile: starting doses are low (e.g., 150 mg/day for smoking cessation) to minimize side effects, with gradual titration typically necessary to reach therapeutic levels. Extended-release formulations provide steady plasma concentrations, optimizing efficacy while limiting peak-trough fluctuations that contribute to discontinuation. Emerging evidence also explores bupropion’s broader applications, including off-label use in managing fatigue, bipolar depression, and even as an adjunct in stimulant use disorder—though such uses remain investigational.
Its versatility underscores a growing appreciation for agents that target neurochemical pathways beyond monoamine reuptake. In real-world practice, bupropion remains a cornerstone of evidence-based care, supported by meta-analyses confirming its superiority over placebo and equivalence to other smoking cessation agents like varenicline and nicotine replacement in certain subgroups. Its non-addictive nature and mood-stabilizing properties make it particularly valuable in patients with comorbid anxiety or bipolar disorder—conditions where other antidepressants may exacerbate symptoms.
As research continues to uncover nuanced pathways in depression and addiction, bupropion’s dual action on norepinephrine and dopamine positions it not merely as an antidepressant, but as a bridge between psychiatric treatment and behavioral intervention. Its distinct classification as an NDRI, coupled with a well-documented safety and efficacy profile, ensures its enduring relevance in modern psychopharmacology—one prescription at a time



Related Post
The Bible Like Never Before: Experience Scripture Through the Audio Majesty of Max Clean Mclean’s Scripture Delivery

Raising Hope Casting: How the Art of Empathetic Storytelling Ignites Change in Media
John Tavaress Wife Aryne Fuller

