Blood Type Discrimination: How Modern Science Revisits Age-Old Myths—and Why They Still Stick
Blood Type Discrimination: How Modern Science Revisits Age-Old Myths—and Why They Still Stick
In a world driven by genetic discovery and diagnostic precision, blood type discrimination has resurfaced as a topic straddling medicine, sociology, and folklore. Once dismissed as pseudoscience, the notion that blood types correlate with personality, health risks, and even social preferences continues to capture public imagination—sometimes with alarming real-world consequences. This persistent fascination stems not from mystery, but from a blend of historical anecdote, emerging research, and the human tendency to seek patterns in complex data.
While blood type’s actual medical role—determining compatibility for transfusions and preventing hemolytic reactions—remains unequivocally established, its role in influencing temperament, disease susceptibility, and lifestyle choices has evolved into a nuanced field of study, demanding careful scientific scrutiny. Blood type discrimination does not emerge solely from outdated stereotypes; it reflects genuine biological variation with measurable, though subtle, effects on health and behavior. The ABO blood group system—defined by the presence or absence of A, B, AB, or O antigens—determines immune responses and interacts with systemic processes ranging from cardiovascular risk to gut microbiome composition.
Beyond transfusion compatibility, researchers have identified links between specific blood types and increased or decreased vulnerability to certain conditions: individuals with non-O types (A, B, AB) show elevated risks for ischemic heart disease, while non-O individuals also demonstrate higher susceptibility to severe complications from infections like COVID-19. These biological truths, however, are frequently misinterpreted or oversimplified in media narratives that conflate correlation with causation. “The scientific record clearly shows that blood type influences disease susceptibility and immune function—this is no longer debatable,” notes Dr.
Elena Marquez, a transfusion medicine specialist at the International Society of Blood Transfusion. “Yet, when this data is stripped of context, it fuels myths about personality clashes or destiny based on type, which lack empirical support.” For instance, long-standing claims that Type O individuals are naturally more disciplined or Type A downs are inherently anxious persist despite no robust clinical validation. “These stereotypes exploit biological plausibility without evidence,” Marquez emphasizes.
“Blood type reflects immune phenotype, not character.” Historically, blood type discrimination gained notoriety during the early 20th century with Karl Landsteiner’s discovery of ABO antigens in 1900, a breakthrough that revolutionized safe transfusions but also laid an unintended foundation for social interpretations. Fast forward to contemporary research, and scientists are now examining how ABO variants may interact with environmental and microbial factors. The Northern European population, for example, exhibits a higher frequency of Type O, a distribution that parallels differential disease patterns across regions—a correlation prompting deeper inquiry into evolutionary pressures.
Recent genome-wide association studies (GWAS) have uncovered intriguing links between blood type genes and traits beyond immunity. Variants in the ABO gene correlate with blood viscosity, clotting factors, and even susceptibility to infections such as Norovirus and malaria—a reflection of evolutionary trade-offs. Non-O individuals often display modifications in their gut microbiome, which may influence metabolism, inflammation, and autoimmune risk.
Yet, these biological nuances are frequently overshadowed by the sensationalism surrounding blood type-based predictions. The allure of blood type discrimination thrives on selective reporting and anecdotal storytelling. Online forums and self-help platforms regularly amplify claims that Type B individuals are inherently intuitive or that Type AB personalities excel in leadership—declarations that lack rigorous validation.
Psychologists attribute this traction to cognitive biases: the human brain excels at pattern detection, and when incomplete data aligns with behavioral stereotypes, confirmation bias strengthens belief. “People treat blood types like fingerprints of identity,” explains Dr. Raj Patel, a behavioral geneticist.
“But genetics alone cannot define personality, resilience, or destiny.” From a medical standpoint, blood type remains a cornerstone of transfusion safety and prenatal screening—predicting Rh incompatibility-related hemolytic disease or guiding Omar blood initial donor matching. Yet, broad claims about blood type dictating learning styles, moral behavior, or career aptitude have no place in evidence-based practice. The danger lies not just in misinformation, but in misuse: insurance companies, employers, or even healthcare providers might unknowingly—or deliberately—leverage such myths, risking discrimination with real-life consequences.
Regulatory bodies and medical associations have taken clear stances. The World Health Organization reaffirms that while ABO genotypes inform medical management, they carry no bearing on temperament or cognitive traits. Similarly, the American College of Chest Physicians emphasizes that blood type discrimination in clinical or social contexts contravenes scientific consensus.
“There is no biological pathway through ABO antigens that shapes behavior, intelligence, or character,” warns Dr. Maria Chen, an expert in genomic ethics. “Honoring genetic diversity means respecting biological reality—not projecting unfounded narratives onto it.” Public engagement with blood type facts remains mixed.
Surveys indicate broad awareness of basic compatibility rules, yet fewer understand the subtle immunological implications. Educational initiatives led by public health institutions now aim to clarify misconceptions, promoting literacy around blood typing as a medical tool rather than a personal identifier. Social scientists caution that eliminating harmful stereotypes requires both scientific transparency and cultural awareness—a dual approach to ensure knowledge empowers rather than divides.
In essence, blood type discrimination sits at the crossroads of fact and folklore—grounded in verified immunology, yet vulnerable to oversimplification. Its medical utility in transfusion, surgery, and prenatal care is indisputable. But as society grapples with identity, health, and data ethics, the line between biological insight and social myth grows fragile.
Only through rigorous, accessible science can the public navigate this complex terrain without being swayed by fading stereotypes or exaggerated claims—ensuring blood type remains a tool for healing, not division.




Related Post

West Memphis 3: DNA Breakthroughs Ignite Fresh Hope in Cold Case DNA Match

October 24th Sign Marked Occasion: A Pivotal Day in Global Humanitarian Commemoration

Hisashi Ouchi: The Human Mirror of Radiation’s Lethal Power
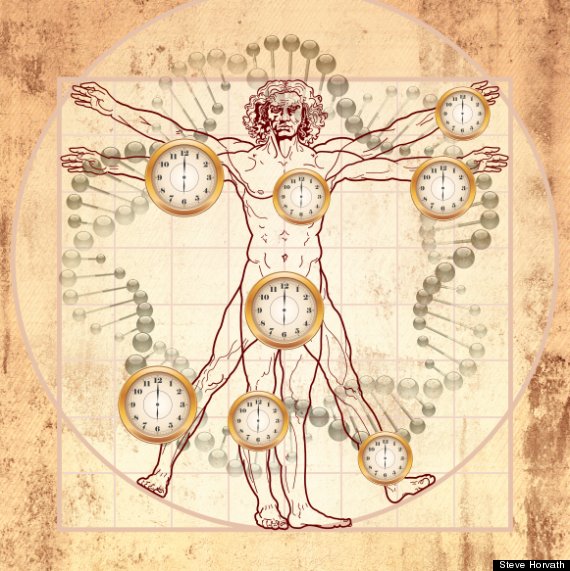
The Jenner’s Ages: Unraveling the Biological Clock and Its Fight Against Time

